This is the Archived Desktop Edition.
This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
Lesson 5: Blood Pressure
5-6
5-6. HOW DO I TAKE A PATIENT'S BLOOD PRESSURE?
Use the following procedures when taking a patient's blood pressure.
a. Gather Materials. You will need the following items:
(1) Sphygmomanometer.
(2) Stethoscope.
(3) Cotton-tipped applicators (swabs)--at least 8.
(4) Disinfecting solution (70% alcohol solution).
(5) Watch or clock with second hand.
(6) Pen or pencil.
(7) Form or note pad on which to write.
b. Verify the Patient's Identity. Make sure that you are preparing to take the blood pressure of the proper person.
c. Set up Equipment. If you have a portable mercury sphygmomanometer, set up the gauge so that it will be at about eye level. If you are using an aneroid gauge, position yourself or the patient so that the gauge will be about eye level when you read it. You can read a gauge easier and more accurately when it is at eye level.
d. Clean Earpieces. Wet one swap with the alcohol disinfecting solution. Clean the inside of one plastic earpiece of the stethoscope with the swab and discard the swab. Wet another swab, clean the outside of the plastic earpiece, and discard that swab also. Repeat the procedure for the other plastic earpiece.
e. Position the Patient. Have the patient to position himself in the desired position.
(1) The blood pressure is normally taken using the patient's upper arm. The patient can stand, sit, or lie down. Normally, the patient will sit with his arm resting on a table or lie down with his arm resting on the bed, cot, or ground.
(2) Sometimes, the physician orders that the patient's blood pressure be taken on his thigh instead of on his arm. (The patient's arms may be injured or amputated, for example.) If the blood pressure is to be taken using the thigh, have the patient to lie on his abdomen. If the patient cannot lie on his abdomen, have him to lie on his back with his knees flexed.
f. Expose the Site. Have the patient expose the site to be used (upper arm or thigh). Assist the patient as needed. The patient may need to remove a long sleeve shirt or lower his pajama bottoms. The bladder must be placed over the patient's flesh, not his clothing. Rolling a shirt-sleeve or pants leg up could create a tight area above the site where the bladder is applied. This extra tightening could cause the blood pressure readings to be inaccurate. Therefore, it is better to remove a long sleeve shirt or pants rather than rolling them up.
g. Explain Procedure to Patient. Briefly tell the patient what you are going to do. The explanation can be combined with instructing the patient to expose the site where the bladder will be applied. Warn the patient that his arm (leg) may be uncomfortable while the bag (bladder) around his arm (leg) is inflated, but reassure the patient that the discomfort will only last 1 or 2 minutes.
h. Prepare Bladder. Make sure that the bladder is completely deflated. If air is present in the bladder, open the release valve, force the air out of the bladder, and close the valve.
i. Prepare Gauge. If a mercury gauge is being used, place the gauge where it can easily read, yet not in the way. If an aneroid gauge is being used, attach it to the bladder.
j. Position Patient's Limb.
(1) If the bladder is to be applied to the patient's upper arm and there is a support for the patient's arm (bed, table, ground, etc.), have the patient to extend his arm in a palm up position. The arm should be about the same level as his heart.
(2) If the bladder is to be applied to the patient's upper arm but there is no support for his arm, tuck his wrist under your arm so that you will be supporting his arm and keeping it steady.
(3) If the bladder is to be applied to the patient's thigh, the patient should remain lying on his abdomen or lying on his back with his knee flexed.
k. Wrap Bladder Around Limb.
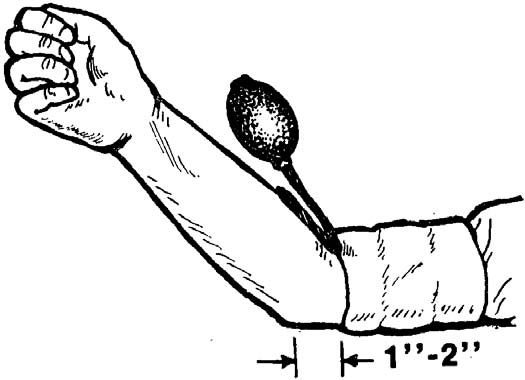
(1) If the upper arm is being used, wrap the bladder around the upper arm. The non-slip material or buckles of the bladder should be on the outside of the bladder, not next to the patient's skin. The bottom edge of the bladder should be one to two inches above the elbow (figure 5-6).
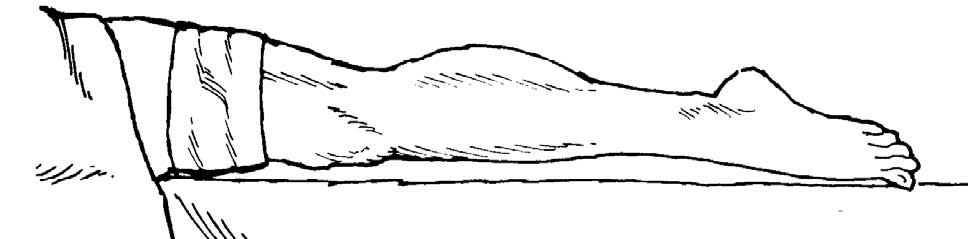
(2) If the thigh is being used, wrap the bladder around the middle of the thigh (figure 5-7). A somewhat larger and longer bladder is normally used when the blood pressure is taken in the thigh.
Figure 5-6. Placement of bladder on upper arm.
Figure 5-7. Placement of bladder on thigh.
(3) Wrap the bladder firmly around the limb. Overlap the fabric and make sure it will not slip (Velcro to Velcro, fasten buckles, tuck fabric end under bladder, etc.).
(4) If an aneroid gauge is being used, wrap the bladder so that the gauge is aligned with the palm of the hand if the arm is used and with the kneecap if the thigh is used. Positioning the gauge in this manner will make it easier for you to read the dial.
l. Locate Pulse. Put the earpieces of the stethoscope in your ears (plastic tips forward) and use the diaphragm to find the patient's pulse.
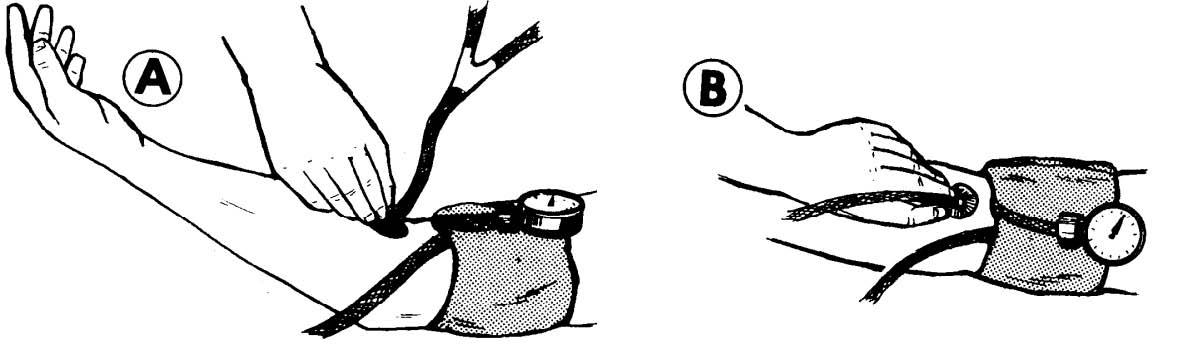
(1) If the upper arm is being used, you will use the brachial pulse found just below the crease on the inside of the elbow (figure 5-8).
Figure 5-8. Locating brachial pulse. A Side view. B Top view
(2) If the thigh is being used, use the popliteal pulse just above the crease on the inside of the knee.
(3) If you are using a combination stethoscope (both disk and bell) and you cannot hear anything, find the lever near the diaphragm and flip it. This will change the source of sound input from the bell to the disk.
m. Tighten Screw. Make sure that the valve is completely closed so that the air cannot escape.
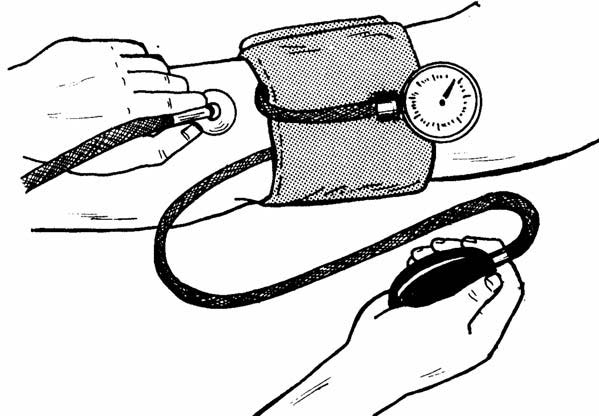
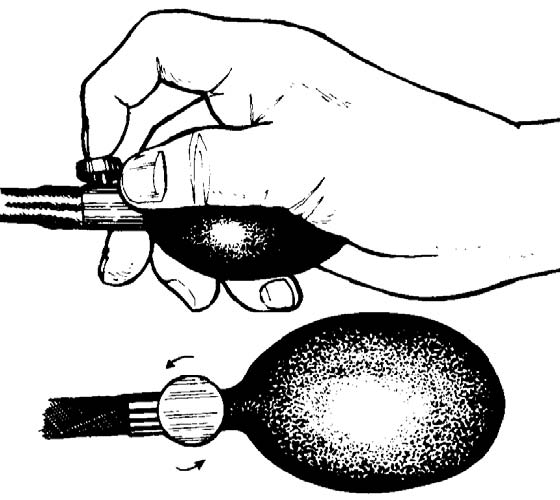
n. Inflate the Bladder. Inflate the bladder (figure 5-9) by squeezing and releasing the handbulb. Listen to the patient's pulse and watch the gauge as you pump up the bladder. When you can no longer hear the pulse beat, note the reading on the gauge. Then pump the handbulb again until it reads 10 mm Hg higher than it did when the pulse disappeared or until the pressure of 140 mm Hg is reached, whichever is greater.
Figure 5-9. Inflating the bladder.
CAUTION: Do not inflate the bladder to a pressure greater than 200 mm Hg. If the
pulse can still be heard at 200 mm Hg, deflate the bladder (unscrew the
valve) and remove the bladder from around the patient's arm or thigh.
Then notify your supervisor of the problem.
o. Listen for Pulse. Once you have inflated the bladder to the desired pressure (140 mm Hg or higher, depending upon when the pulse disappeared) listen briefly to make sure that you cannot hear the pulse beat below the bladder.
(1) If you cannot hear the pulse, then the air pressure inside the bladder is greater than the systolic pressure of the blood. (The bladder is, in effect, now a tourniquet.) You are now ready to begin releasing the air from the bladder.
(2) If the pulse can still be heard, inflate the bladder until the pulse disappears, then inflate it an extra 10 mm Hg of pressure. Do not inflate above 200 mm Hg.
p. Release Air Slowly. Watch the gauge closely and listen through the stethoscope as you release air from the bladder. Air is released from the bladder by rotating the release valve (screw) counterclockwise (figure 5-10). The more the screw is turned, the larger the opening and the faster the air escapes. You want the air to escape slowly enough so that you can tell at what pressure reading the pulse reappears, but fast enough that the continued pressure does not harm the patient or cause unnecessary discomfort.
Figure 5-10. Rotating the screw counterclockwise to release pressure.
(1) The process of taking a patient's blood pressure (beginning at the time you start inflating the bladder and ending at the time you completely release the pressure) should take less than two minutes. Do not leave an inflated bladder wrapped around the patient's limb for more than two minutes.
(2) If you are having problems that will result in going over the two minute mark, deflate the bladder, remove the bladder from around the patient's limb, and wait at least one minute before trying to take his blood pressure again.
q. Listen for Pulse. The point at which you hear the pulse beat return is the patient's systolic pressure. Note the reading on the gauge when you hear the first distinct sound of a pulse beat.
(1) The markings on the gauge will mark off readings (130, 132, 134, etc.). When you record blood pressure readings, record the reading to the nearest even number (for example, 128 instead of 127).
(2) Normally, you will remember the patient's systolic reading and not write it down until you have the determined his diastolic reading also. Writing the number down distracts you from listening to the pulse and watching the gauge as the air continues to escape.
r. Continue to Release Pressure. After you identify the patient's systolic pressure, continue to listen to the pulse and watch the gauge as the air continues to escape from the valve. The air should be escaping at a rate that does not require you to adjust the airflow (turn the screw).
s. Listen for Last Distinct Sound. As long as the air pressure in the bladder is greater than the diastolic pressure, the artery will collapse after each pulse beat. This makes the pulse have distinct sound. Once the air pressure in the bladder is less than the diastolic pressure of the blood, the artery will remain open at all times. This means that you will be hearing the sound of continuous blood flow in addition to the blood surge caused by the pulse. The pulse will sound muffled and not distinct. The point at which the distinct pulse sound changes to a muffled sound marks the diastolic pressure.
(1) Often the pulse will sound louder just before the diastolic pressure is reached.
(2) A change in rhythm may also occur at the diastolic level.
(3) Sometimes the diastolic is difficult to determine. You may wish to close the valve (turn screw clockwise), inflate the bladder to a point where the pressure is above the diastolic, and release the air at a slower rate than before in order to check yourself.
(4) Like the systolic, the diastolic is determined to the nearest even whole mm Hg.
t. Release Air. Once you have determined the patient's diastolic pressure, rotate the screw counterclockwise until the valve is opened as far as possible. This will allow the bladder to deflate rapidly.
u. Verify Readings, if Needed. If you are not sure that the blood pressure readings (both systolic and diastolic) are correct, squeeze all the air out of the bladder while it is still wrapped around the patient's arm and repeat steps m through t. The blood pressure can usually be checked quickly because you already know the patient's approximate blood pressure readings. This means that you will usually inflate the bladder quickly to a pressure about 10 mm Hg above the first reading, release the air slowly until the first pulse is heard, release air little faster, and then slow the air flow down when you approach the level of the diastolic reading. If the second set of readings is very different from the first, remove the bladder from the patient's limb, force the remaining air out, wait one minute, and take his blood pressure again.
v. Record Readings. Record the systolic and diastolic readings. The systolic is written first and is separated from the diastolic by a diagonal line. For example, a systolic of 120 and a diastolic of 80 is written "120/80." Both reading are recorded as whole, even numbers.
w. Remove Bladder. Remove the bladder from around the patient's arm or thigh, force the remaining air out of the bladder, and close the valve.
x. Assist Patient, If Needed. Assist the patient as needed. For example, you may need to help the patient with his shirt or pajamas.
y. Clean Earpieces. If you are not going to continue using the stethoscope, clean the earpieces again. Use the same procedures as previously described in paragraph d.
z. Return Equipment. If you will no longer need the sphygmomanometer and stethoscope, return them, along with any other equipment used, to their proper storage area.