Special Surgical Procedures II
LESSON 2: Procedures in Gynecological and Obstetrical Surgery
Section Ii:
2-15
2-15. VAGINAL PLASTIC OPERATION (ANTERIOR AND POSTERIOR REPAIR)
a. General.
(1) This operation involves reconstruction of the vaginal walls, the pelvic floor, and the muscles and fascia of the rectum, urethra, bladder, and perineum. It involves a vaginal repair to correct a cystocele and/or rectocele, restore the bladder to its normal position, and strengthen the vagina and the pelvic floor.
(2) A cystocele is formed when the portion of the anterior vaginal wall that is between the cervix and the urethra and the base of the bladder herniate inferiorly. The hernia of the bladder protrudes through the torn musculofascial components of the vaginal anterior wall, with protrusion into the vaginal outlet. A defect in the anterior vaginal wall is usually caused by childbirth or an inherent weakness. A large herniation may cause a sensation of pressure in the vagina or present as a mass at or through the introitus.
(3) A rectocele is formed by a herniation of the anterior rectal wall (posterior vaginal wall) into the vaginal outlet. In general, the anterior rectal wall forms a bulging mass beneath the posterior vaginal mucosa. It is created as the mass pushes downward into the lower vaginal canal. The rectum, may be torn from its dense connective tissue, the fascial and muscular attachments of the urogenital diaphragm, and the pelvic wall. The levator ani muscles become stretched or torn. The symptomatic signs are a mass protruding from the vagina, difficulty in evacuating the lower bowel, and a feeling of pressure.
(4) An enterocele is a protrusion of the cul-de-sac of Douglas and some of the pelvic small intestine within the peritoneal sac. It pierces through a weakened area between the attenuated anterior rectal and posterior vaginal walls.
(5) An enterocele may also be seen in multiparous women as part of a massive lesion, in which a large sac contains the bladder, lower portions of the ureters, and the prolapsed uterus. In some cases, a Kelly or Marshall-Marchetti operation may be necessary to treat urinary incontinence and uterine prolapse.
(6) During parturition, the outer fibrous layers of the vagina may be torn, thereby permitting the adjoining viscera to herniate into the vaginal outlet. Because of unrepaired perineal lacerations, gradual pulling apart of the underlying fascia and muscles of the pelvic floor and outlet takes place. The woman has symptoms of relaxation and displacement of the pelvic organs. Accidents, gradual deterioration of tissues, or congenital weakness, may also result in mechanical disturbances of the pelvic structures.
b. General Operative Procedure. Dilatation and curettage may be done. The labia are held open with retractors and the cervix is grasped with a tenaculum. Adair forceps are used to retract the cervix; self-retaining or Sims retractors are used to expose the operative site.
c. Anterior Wall Repair.
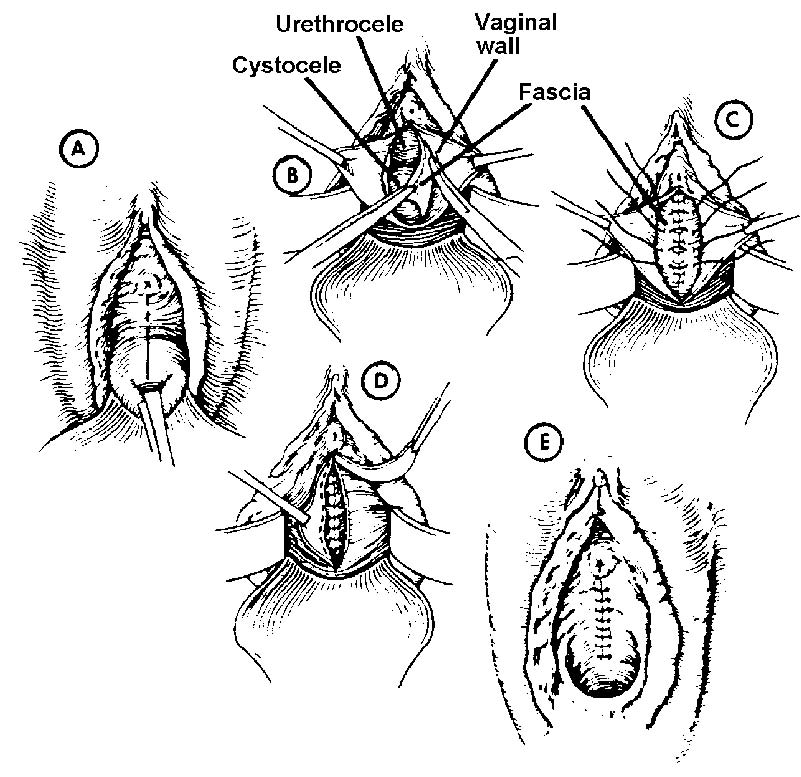
(1) Areolar tissue between the bladder and vagina at the bladder reflection is exposed with the knife handle. The full thickness of the vaginal wall is separated up to the bladder neck, using a knife, curved scissors, tissue forceps, Adair or Allis forceps, and sponges on holders. Bleeding vessels are clamped and tied with ligatures (see figure 2-5 A).
(2) The urethra and bladder neck are freely mobilized, using a knife, gauze sponges, and curved scissors (see figure 2-5 B), to develop the strong free edge of, the vesicovaginal fascia on each side.
(3) The free edges of the fascia are sutured, using chromic gut sutures number2-0. Sutures are placed in a manner that after they have been tied, there results a double inverting of the tissue, a narrowing of the bladder neck, and a delineating of the posterior ureterovesical angle (see figure 2-5 C).
(4) The connective tissue on the lateral aspects of the cervix is sutured into the cervix with chromic gut number 2-0 sutures swaged on curved needles. This is done to shorten the cardinal ligaments.
(5) Allis forceps are applied to the edges of the incision, and the left flap of the vaginal wall is drawn across the midline. Edges are trimmed according to the size of the cystocele (see figure 2-5 D). This process is repeated on the right flap of the vaginal incision. Adair forceps, tissue forceps, and curved scissors are needed.
(6) The anterior vaginal wall is closed with interrupted chromic gut number 2-0 sutures in a manner resulting in reconstruction of an anterior vaginal fornix.
d. Posterior Wall Repair.
(1) Allis forceps are placed posteriorly at the mucocutaneous junction on each side, at the hymenal ring, and just above the anus.
(2) Skin and mucosa are incised and dissected from the musculature beneath, using a knife, tissue forceps, curved scissors, and sponges.
(3) Allis-Adair forceps are placed on the posterior vaginal wall, scar tissue is removed, and dissection is continued to the posterior vaginal fornix and laterally, depending on the size of the rectocele.
(4) The perineum is denuded by sharp dissection; the trimming of the posterior vaginal wall is carried out, using Allis forceps, curved scissors, and sponges on holders.
(5) The free edges of the levator ani muscle on each side are brought together in front of the rectum by insertion of interrupted chromic gut number 0 sutures.
(6) Bleeding is controlled, and the vaginal wall is closed from above downward to the anterior edge of the puborectal muscle, using continuous chromic gut number2-0 suture. The rectocele is repaired from the posterior fornix to the perineal body. Remains of the transverse perineal and bulbocavernosus muscles are used to build up the perineum. The anterior edge of the levator ani sling may be approximated.
(7) The mucosa and skin are trimmed, and the remaining closure is effected by interrupted sutures. The skin is closed with subcuticular sutures, chromic gut number 2-0.
(8) The vagina is packed with 2-inch vaginal packing. An indwelling urinary drainage system is established. A perineal pad may be applied to the wound and held in place by means of a perineal binder.
Figure 2-5. Correction of cystourethrocele.
|
A-Cervix pulled down as far as possible with tenaculum. Vertical incision made entirely through to vaginal wall.
B-Vaginal flaps further dissected upward. Urethral meatus and pubocervical fascia separated from vaginal wall with Mayo scissors.
C-Fascia brought together with continuous surgical chromic suture, beginning at lowest point and ending near external urethral meatus. A few interrupted sutures (chromic gut or silk) placed secondarily.
D-Excess portion of vaginal wall carefully removed, leaving sufficient amount to be closed with tension.
E-Completed operation, maintaining bladder and urethra in normal position. |