Integumentary System
Lesson 1: Anatomy and Physiology of the Integumentary System
1-3
1-3. APPENDAGES ASSOCIATED WITH THE SKIN
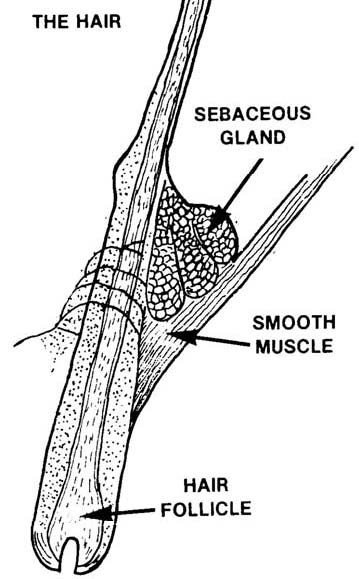
a. Hair. See figure 1-3.
(1) General information. Hairs, growths of the epidermis, are distributed over various parts of the body. The primary function of hair is to protect. Hair on the head protects the scalp from injury and sunburn. Eyelashes and eyebrows protect eyes from foreign matter. Hair in the nostrils and external ear canal protects from insects and dust. Hair is a keratinized structure that grows out of a tubular canal called a hair follicle.
(2) Distribution. Nearly all parts of the body have hair. An average adult probably has about five million hairs, about 100,000 of these on the scalp. Straight hairs are oval or cylindrical in cross section while a cross section of curly hair shows it flattened. Straight hairs are stronger than curly hairs.
(3) Structure. A shaft and a root make up each hair.
(a) Shaft. The hair shaft is the superficial part of the hair that sticks out above the skin surface. A course hair shaft has three parts: the inner medulla, the middle cortex, and the outermost layer, which is the hair cuticle. Polyhedral cells with granules of eleidin and air spaces make up the medulla. (The medulla may or may not be present in fine hair.) The cortex is the major part of the hair shaft and has cells that contain pigment in dark hair. These cells are mostly air in white hair. The cuticle, the outermost layer of the shaft, is composed of one layer of thin, flat, scale-like cells that are heavily keratinized.
(b) Root. The hair root is the portion below the skin surface. The root is embedded in the epidermis and penetrates the dermis and the subcutaneous layers of skin. The root also contains a medulla, cortex, and cuticle. The hair follicle, surrounding the root, is made up of an external root sheath and an internal root sheath (both composed of epithelium).
(c) Bulb. An enlarged, onion-shaped structure called a bulb is at the base of each hair follicle. The bulb contains the papilla of the hair, an indentation filled with loose connective tissue. The papilla of the hair contains many blood vessels and provides nourishment for the growing hair. There is a region in the bulb called the matrix. When older hairs are shed, matrix cells produce new hairs by cell division. The replacement occurs within the same follicle that lost a hair.
Figure 1-3. Principal parts of a hair.
(d) Arrector pili. The arrector pili are bundles of smooth muscle that extends from the dermis of the skin to the side of the hair follicle. Normally, hair is at an angle to the surface of the skin. Under stress, from fright or cold, for example, the arrector pilorum muscles contract and pull the hairs into a vertical position. The result is "goosebumps" or "gooseflesh" because the muscle contraction has made the skin around the hair shaft rise a little.
(4) Color. A substance called melanin is responsible for hair color. Melanocytes in the matrix of the bulb of the hair follicle form melanin. Hair pigment exists in three colors: yellow, brown, and black. Yellow comes from pheomelanin, brown pigment from brown melanin, and black pigment from black melanin. Combinations of different amounts of the three pigments make for
variations in hair color. Graying hair is the result of the loss of hair pigment. The cause is thought to be a progressive inability of the melanocytes to make tyrosinase, the enzyme necessary for the synthesis of melanin. Air in the medullary shaft causes white hair.
(5) Hair growth and replacement. There is a cyclic pattern-- alternating growing and resting periods--to hair growth and replacement. The matrix cells are active during the growing phase when these cells divide thus increasing their number, push upward, and eventually die. A hair, dead protein tissue, is the product. Hair grows about 1 mm (0.04 inch) every three days. During the resting phase, the matrix is inactive, and these cells shrink causing the hair root to detach itself from the matrix and the hair to move up the hair follicle slowly. The hair may stay in this position for a while until it is pulled out, shed, or pushed up by a replacing hair. The cycle of hair growth is different in different parts of the body. Scalp hair grows steadily and continuously for two to six years. Growth stops, and after three months, the hair is shed. Three months later a new hair starts to grow from the same follicle. On the other hand, eyebrows have a growing phase of only about ten weeks, which is why eyebrow hair is not very long.
b. Nails.
(1) Parts of the nail. Nails are hardened, horny-like epidermal cells. These cells form a clear, solid covering over the back surfaces of the fingers and toes. Each nail has three parts: nail body, free edge, and nail root. The part of the nail you can see is the nail body. The free edge is the part of the nail that extends beyond the finger or toe, and the nail root is the part of the nail that is hidden in the nail groove. Tissues under the nails have many blood vessels, which accounts for the fact that the nail body appears to be pink. The whitish, moon-shaped area near the nail root is the lunula. It is whitish in color due to tissues with blood vessels that do not show through. The nail fold is the fold of skin around the borders of the nail. The skin beneath the nail is the nail bed.
(2) Growth of the nail. Nail growth takes place in the part of the nail under the body and nail root. Superficial cells in the matrix change into nail cells, and the outer, harder nail layer is pushed forward making the nail longer. Fingernails grow at a rate of approximately 1 mm (0.04) per week while toenails grow a little more slowly. It takes approximately three and a half to five and a half months for a lost fingernail to regrow. A lost toenail takes a little longer--six to eight months.
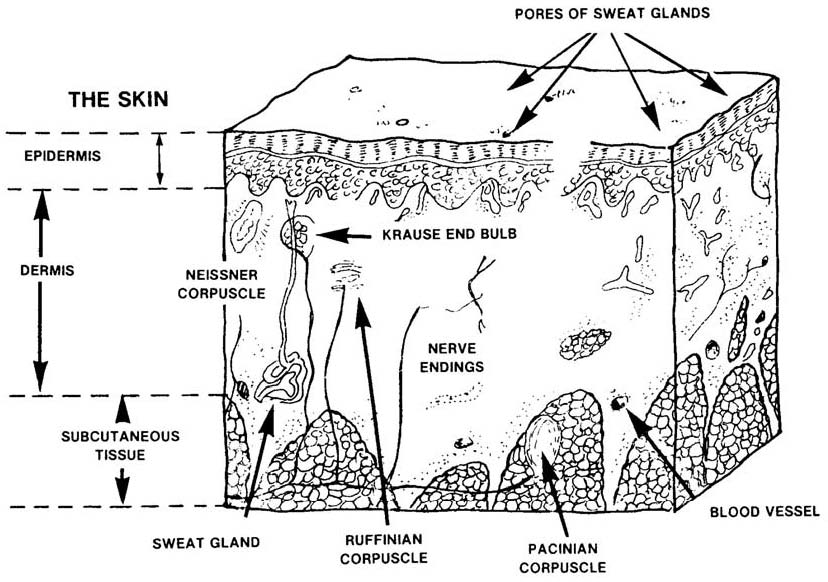
c. Skin Glands. These are the three kinds of skin glands: sebaceous glands; sweat glands (sudoriferous glands); and modified sweat glands. See figure 1-4.
(1) Sebaceous glands. These glands, not found in the palms of the hands or the soles of the feet, are oil glands that are connected to hair follicles. The glands are in many parts of the body and exist in a variety of shapes and sizes. Sebaceous glands secrete a substance called sebum, an oily substance that is a mixture of fats, cholesterol, proteins, and inorganic salts. Sebum acts as a skin lubricant keeping hair from drying and becoming too brittle. This substance also forms a protective film that prevents too much water from evaporating from the skin; this protective film is responsible for the skin being soft and pliable. More sebum is produced in puberty, while less sebum is produced in old age. Sebum has antifungal and antibacterial properties. If too much sebum accumulates in the sebaceous glands of the face, causing these glands to get bigger, blackheads can develop. The air oxidizes the sebaceous gland fatty material discoloring that fatty substance, hence blackheads. If fatty substances accumulate in the sebaceous glands, pus-producing bacteria in those substances can cause pimples to form. The skin problem acne is an inflammation of sebaceous glands. A few blackheads or whiteheads on the face may be a sign of approaching puberty.
Figure 1-4. Skin glands.
(2) Sweat glands (sudoriferous glands).
(a) Characteristics. There are two principal types of sweat glands: apocrine sweat glands and eccrine sweat glands. Both are simple, tubular glands distributed throughout the skin. One difference is that apocrine sweat glands are branched and eccrine sweat glands are coiled. Another difference is that apocrine glands are located in the axilla, pubic region, and pigmented areas of the breasts. The eccrine glands are located throughout the body except in the margins of the lips, nail beds of fingers and toes, and the eardrums. Eccrine sweat glands are most numerous in the skin on the palms of the hands and the soles of the feet. Sweat gland density in the palms of the hands can be as high as 3,000 glands per square inch.
(b) Secretion. The part of the apocrine gland that secretes sweat is located in the dermis; for eccrine glands, that portion of the gland is in the subcutaneous layer of skin. The substance secreted by both types of sweat gland is perspiration or sweat. Pure sweat contains much the same elements as blood, but in lower concentrations. The chief element is water, then sodium chloride, potassium, glucose, ureas, and lactate. Pure sweat is odorless. Odor comes from sweat interacting with bacteria on the skin.
(c) Function. The principal function of the sweat glands is to help regulate body temperature. Sweating can cool the body because body heat is necessary for the water in sweat to evaporate. The amount of water lost by sweating can be as much as eight pounds of body weight per day. The function of apocrine glands is to respond to emotional stimulation.
(3) Modified sweat glands.
(a) Ceruminous (wax) glands. In some parts of the skin, sudoriferous glands are modified and become ceruminous glands. These are simple, coiled, tubular glands located in the external meatus of the ear canal. The substance secreted is wax, also called cerumen. This substance may accumulate resulting in too much earwax. The combination of hair and earwax helps prevent foreign objects from entering the ear.
(b) Ciliary glands. These glands are located on the edges of the eyelids. The glands secrete a milky, alkaline sweat. The function of the sweat is to moisten the inner eyelids.