Integumentary System
Lesson 3: Primary and Secondary Skin Lesions
3-4
3-4. TYPES OF SKIN LESIONS
a. General Information. Generally, while the epidermis plays a leading role in the skin by being the barrier between the human's internal tissues, and so forth, and the environment, the dermis is the more indispensable. Of the two layers, the dermis is much thicker and measures up to four mm in depth. The dermis is composed of collagenous and elastic tissues. These tissues provide the structural base for the epidermis as well as a site for vascular and nerve networks in the skin. Alteration in any component of the skin-- epidermis, dermis, or any skin appendage--can result in clinically visible skin lesions.
b. Types of Skin Lesions. Skin lesions can be divided into three categories: primary skin lesions, secondary skin lesions, and special skin lesions. Primary skin lesions are basic and simple. Secondary skin lesions result from complications of primary skin lesions.
c. Primary Skin Lesions.
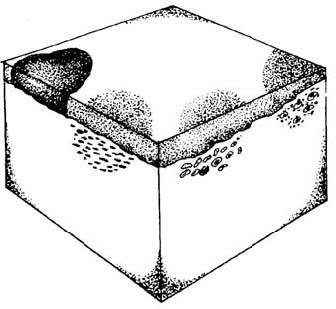
(1) Macule. A macule (figure 3-3) is a definite area of skin in which the skin color has changed from the normal skin color. This area is neither higher nor lower than the surrounding skin area. These flat, discolored spots are either hypopigmented (abnormally diminished in pigmentation) or hyperpigmented (abnormally increased in pigmentation). The lesions are of varied size, less than one milliliter in diameter. Macules may be adjacent to each other and cover a whole extremity (for example, a leg) or half of the face (as in the disease capillary hemangioma). Macules may be cafe au lait colored (color of coffee with milk) as in Albright's syndrome, blue to black as in urticaria (hives), or white as in certain forms of leprosy.
Figure 3-3. Macule.
(2) Papule. A papule (figure 3-4) is a solid, elevated lesion usually 0.5 cm to 1 cm or less in diameter. Most of the lesion is above the level of the surrounding skin rather than deep within the skin. Many skin diseases start with papules--warts, psoriasis, syphilis, drug eruptions, and some phases of acne. Different types of papules are different colors. The papules of psoriasis are flat-topped and red, often with a superimposed scale that produces bleeding when removed. Skin lesions of a secondary syphilis are copper colored. Violet papules are typical of lichen planus skin lesions, and the papules of lichen sclerosis are whitish. Rounded, red, bluish-red, or brownish-red papules characterize the skin disease pyogenicum.
Figure 3-4. Papule.
(3) Nodule. A nodule (figure 3-5) is a solid, elevated lesion that extends deeper into the dermis than the papule. A nodule is greater than 0.5 cm in diameter but less than 2 cm and may or may not be elevated above the level of the surrounding skin. Examples of nodules include keratinous cysts, small lipomas (benign tumors composed of mature fat cells), fibromas (benign tumors derived from fibrous connective tissue), some types of lymphoma (malignant diseases usually in the lymph nodes), and a variety of neoplasms (abnormal, excessive, and uncontrolled multiplication of cells forming a mass or new growth of tissue). Nodules are often an indication of systemic disease and can result from inflammation, neoplasms, or metabolic deposit in the dermis or subcutaneous tissue. For example, nodules are present in late syphilis, tuberculosis, and roundworm infestation. Sometimes local agents can produce nodules--foreign-body reactions, milker's virus, or tick bites.
Figure 3-5. Nodule.
(4) Tumor. A tumor is an elevated, solid lesion greater than 2 cm. Tumor, a general term for any mass, benign or malignant, is sometimes used to indicate a large nodule. The skin is an extremely common site for a wide variety of tumors; most are easily visible in the earliest stages. Therefore, it is possible to recognize and eradicate tumors in almost 100 percent of the cases. The following are a few of the origins of skin tumors: tumors arising from the epidermis surface; tumors arising from epidermal appendages such as hair structures, sebaceous glands, and sweat glands. Examples of common skin tumors are actinic keratoses, usually caused by repeated exposure to sunlight over the years. These tumors are frequently noted in
middle-age sailors, sportsmen, and farmers. Actinic keratoses are more common in the Southwestern US than in areas with less sunlight. Fair-skinned people are more susceptible to these tumors than those with dark skin. People who are bald frequently develop multiple actinic keratoses.
(5) Wheal. A wheal (figure 3-6) is an elevated lesion (rounded or flat-topped). A wheal has increased tissue fluid, often itches, and usually disappears within a few hours. Trace the wheal with a skin marking pencil, observing over a period of time. You will see the lesions shift rapidly from involved to uninvolved adjacent skin areas. The lesions are the result of excess fluid in the upper layer of the dermis. Wheals are pale red and may be an allergic response to any one of a number of irritants or to insect bites. Twenty-five percent of the normal population can produce wheals merely by stroking their skin. This phenomenon is called dermatographism. The size of wheals varies from 3 to 4 mm in diameter as in the skin disease cholinergic urticaria or 10 to 12 mm as in the skin diseases composed of erythematous plaques.
Figure 3-6. Wheal.
(6) Plaque. A plaque (figure 3-7) is a rather large surface area which is elevated above the surrounding skin surface. In the skin disease psoriasis, a number of papules form the plaque. In the skin disease lichenification, the skin on the plaque appears thickened, and the skin markings are more visible than usual. Also, the surface of the skin lesions may resemble tree bark. Lichenification is caused by repeatedly rubbing a skin area.
Figure 3-7. Plaque.
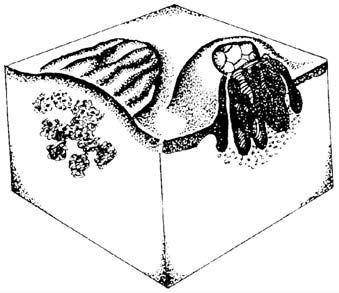
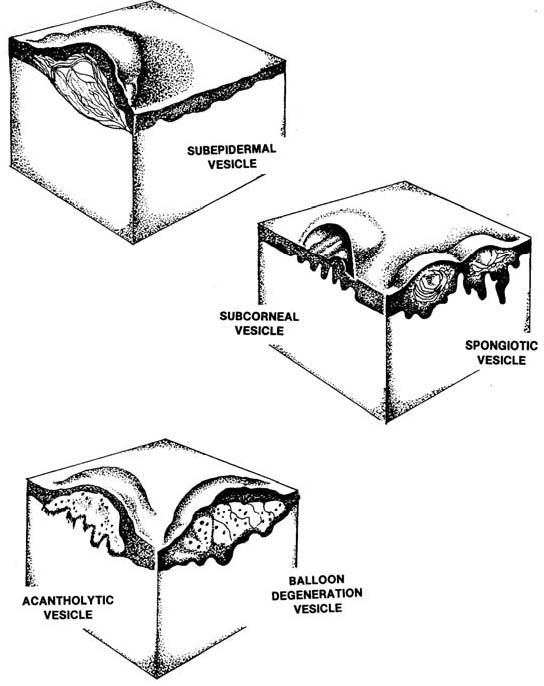
(7) Vesicle and bulla. A vesicle (figure 3-8) is an elevated, fluid-filled skin lesion that is less than 0.5 cm in diameter. A bulla is the same as a vesicle with the exception that the bulla is greater than 0.5 cm in diameter. A vesicle or bulla arises from a cleavage at various levels of the skin. When the cleavage is just beneath the stratum corneum of the skin, a subcorneal vesicle or bulla results as in impetigo and corneal pustular dermatosis. Sometimes the vesicle or bulla walls are so thin that you can see through them. In such instances, the serum, lymph, blood, or extracellular fluid is quite visible.
Figure 3-8. Types of vesicles.
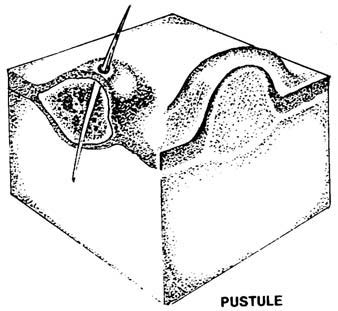
(8) Pustule. A pustule (figure 3-9) is a pus-filled lesion that can result from infection of vesicles or bullae. The pus is a thick fluid composed primarily of dead white blood cells (leukocytes) and a thin liquid and often the microbiologic agent responsible for the inflammation. The pustule may appear white, yellow, or greenish-yellow, depending on the color of the material being deposited in the tissue. An example of a common pustule is a follicular or hair pustule. Hair pustules are usually shaped like a cone, have a hair in the center, and heal without scarring.
Figure 3-9. Pustule.
d. Secondary Skin Lesions. Secondary lesions are the result of some primary lesion. A number of conditions such as crust and scale are characteristic of secondary lesions.
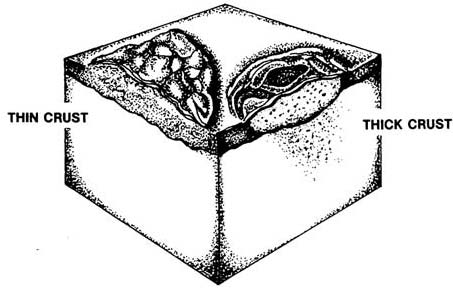
(1) Crust. The dried residue of fluid, blood, or pus on an area of lost or damaged skin surface is crust (figure 3-10). Crusts may be thin, delicate, and easily torn or damaged or the crust may be thick and sticking to the skin. Crusts formed from dried serum (the clear fluid of blood) are yellow while crust formed from pus are yellow-green, and crusts formed from blood are dark red or brown. When dealing with crust, it is most important to determine what is underneath the crust--dermatitis, superficial infection, or ulcer.
Figure 3-10. Crust.
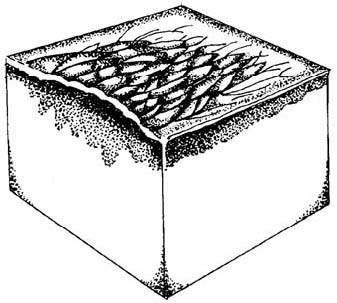
(2) Scales. Scales are a buildup of dry cells (horny layer) that is higher than usual. Although there are a large variety of scales, some are so distinctive that they can be used to diagnose specific skin problems. For example, a chronic plaque-like scale that is silvery-white to gray is usually psoriasis. Greasy, yellowish scales may indicate seborrheic dermatitis. If the scales are dry and diffuse and look like fish scales on the lower legs, the skin disease is icthyosis. Skin lesions of pityriasis rosea and tinea corpis scale mainly at the edge of individual lesions.
(3) Fissure. A fissure is a crack in the epidermis extending into the dermis. They are linear cleavages in the skin, sometimes very painful. These cracks occur particularly in the hands and feet, especially after therapy has caused excessive drying of the skin. Fissures also occur at the angles of the mouth.
(4) Erosion. A loss of epidermis that does not extend into the dermis is termed erosion. Erosion is often seen in herpes infections.
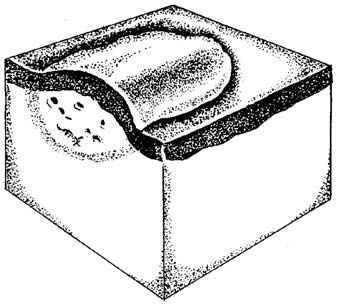
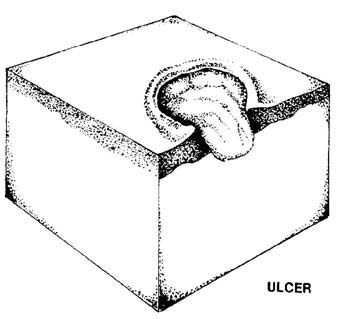
(5) Ulcer. An ulcer (figure 3-11) is a skin lesion in which there has been destruction of the epidermis and the upper papillary dermis. An ulcer always results in a scar. To determine the cause of an ulcer, note the ulcer's location, borders, base, discharge, and any associated features of the lesion such as nodules, excoriations (scratch marks), varicosities (abnormal swellings), hair distribution, presence or absence of sweating, and adjacent pulses. There are many causes of ulcers--skin trauma of all kinds (heat, cold, electrical, chemical); bacterial, viral, and fungal infections; parasitic infestations; and tumors to name just a few.
Figure 3-11. Ulcer.
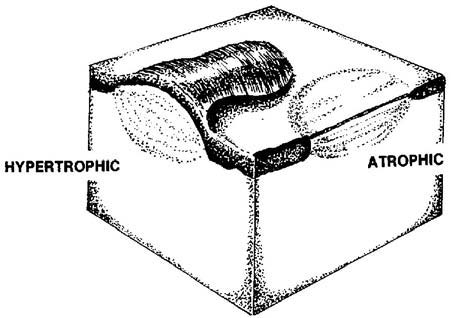
(6) Scar. A scar (figure 3-12) is a fibrous healing of a wound, healing that replaces the normal dermis and epidermis that have been damaged. Scars in different areas of the body may look different. Hypertrophic scars (scars with excessive fibers) result when a lot of collagen is produced in the healing process. This type of scar may occur in the course of acne, herpes zoster, and porphyria (a disorder of blood pigment metabolism). In atrophic scars, the epidermis is thin and usually has neither skin lines nor appendages. This type of scar may be depressed.
Figure 3-12. Scar.
(7) Keloid. A keloid appears in an area of injury or just arises spontaneously; it is a smooth overgrowth of fibroblastic tissue (tissues composed of spindle-shaped cells). A typical keloid is first noticeable as a small, fairly firm nodule and slowly becomes a marked, several-lobe mass of a dark brown color. The keloid has spontaneous burning, itching, and tingling. Keloids are more frequent in blacks.
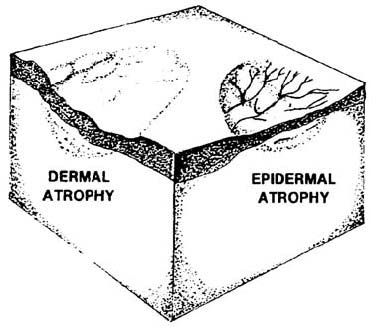
(8) Atrophy. Skin atrophy (figure 3-13) is a thinning and wrinkling of the epidermis often seen in the aged. Another type of skin atrophy is the stretch marks seen in the skin of women who have been pregnant or in the skin of people who have had a large weight loss. Glistening white bands in the skin are typical of these stretch marks, the bands having been caused by overstretching and weakening of the elastic tissue of the skin.
Figure 3-13. Atrophy.
e. Special Skin Lesions.
(1) Comedo (blackhead). A comedo or blackhead develops when sebaceous glands become enlarged because of accumulated serum. Blackheads more commonly happen during adolescence and are usually found over the face, chest, and back. The color of blackheads is caused by melanin and oxidized oil, not dirt. A blackhead is of cosmetic rather than medical importance. The contents of the lesion may be removed with an extractor that takes out the plug and improves cosmetic appearance. Often, however, the blackhead returns in full flower within a month.
(2) Milia (whitehead). A milia or whitehead occurs when a sebaceous duct is blocked with horny materials. These skin lesions, of cosmetic importance only, are small, superficial, keratinous cysts. To remove these cysts, make a small opening with a scalpel and remove the cyst with a comedo extractor.
(3) Sebaceous cyst. A sebaceous cyst forms as a result of a blocked sebaceous duct which continues its activity. In puberty, the growth-pattern of sebaceous glands changes often cause an increase in sebaceous cysts.
(4) Wen. A wen is a common type of epidermal cyst, a sebaceous cyst, found on the scalp or scrotum. This type of sebaceous cyst is a slow-growing cyst containing follicular, keratinous, and sebaceous material. When palpated, the cystic mass is firm, globular, moveable, and nontender. It seldom causes discomfort unless it is infected. When punctured, the contents of the cyst are found to be cheesy, often fetid formed of epithelial debris and greasy material with soft keratin present. Sometimes, calcium deposits may be found. If the wen is small, the contents may be expressed by making a tiny stab incision. If the wen is large, a small incision can be made and the contents evacuated. Then, remove the cyst wall with a curette or hemostat. The wall of a large cyst must be removed to prevent recurrence of the cyst.
(5) Folliculitis (ingrown hair). Usually caused by Staphylococcus
aureus, folliculitis is a superficial or deep bacterial infection and irritation of the hair follicle. The lesion is made up of a superficial pustule or inflammatory nodule surrounding a hair. Infected hairs can be easily removed. When the hair follicles are deep in the skin (for example, the bearded region), folliculitis may become chronic. Stiff hairs in the bearded area of the skin may come out of the hair follicle, curve, and reenter the skin. This produces a chronic, low-grade irritation without major infection. To prevent folliculitis, aggravating factors or irritations must be corrected.
(6) Furuncle (boil). A furuncle is a deep-seated infection with a single core; the infection involves the entire hair follicle and adjacent subcutaneous tissue. This lesion becomes a pustule 5 to 30 mm in diameter with central necrosis that discharges a core and liquid. Furuncles usually occur in hairy parts of the body where there is irritation, friction, pressure, moisture, or oily skin. Although furuncles occur frequently on the neck, breasts, face, or buttocks, these skin lesions are most painful when they occur in skin that is closely attached to underlying structures; for example, the nose, ear, or fingers. Furuncles can occur over and over, often in healthy young people.
(7) Carbuncle. A carbuncle is a staph infection with multiple tracts (several furuncles) that extend into the subcutaneous tissue. The furuncles have developed in adjoining hair follicles, developing more slowly than one furuncle and sometimes accompanied by fever and prostration. The infection causes pus to be produced and drain from the furuncles. Carbuncles develop most frequently in males occurring commonly on the nape of the neck.
(8) Abscess. An abscess is a localized collection of pus, usually caused by bacterial infection, in tissues, organs, or confined spaces. Abscesses in cutaneous or subcutaneous skin layers are evident by swelling, tenderness, and redness over the affected site. The patient may experience fever if the infection is spreading. Usually, the contents of an abscess must be removed for healing to take place. The abscess sometimes ruptures spontaneously into adjacent tissue or outside the body.
(9) Telangiectasia. This skin lesion is a small cluster of dilated blood vessels. Fine, bright red lines or net-like patterns may be seen on the skin. Usually not elevated, these skin lesions can be found around the nail bed, on the face and trunk. Telangiectases are common on the face of people who are in the sun and wind a great deal.
(10) Petechiae. A petechia is a small hemorrhage under the skin. This lesion appears as a nonraised, purplish-red spot on the skin, nailbeds, or mucous membranes.
(11) Ecchymosis. This is a ruptured vein commonly called a bruise. It is a black and blue spot on the skin caused by the escape of blood from injured blood vessels.
(12) Maceration. Maceration is a softening of solid tissue by soaking. The tissue turns white and breaks down easily.
(13) Burrow. A burrow is a tunnel or linear train in the epidermal layer of the skin caused by a parasite. The contagious, parasitic skin disease scabies is a good example of a parasite burrowing. The skin damage is caused by the female Sarcoptes scabiei who excavates a burrow in the stratum corneum layer of the epidermis, lays her eggs and dies. The larvae emerge, moult, and the females are fertilized. The most common sites in which the parasite enters the skin are between the fingers, the hands, and the wrists. The infection can persist for months or years if a person is not treated, a situation which gave rise to the expression "the seven-year itch."
(14) Excoriation. Loss of skin due to scratching is called excoriation. The implication is that the person has scratched himself, but the scratch mark can also be of unknown origin.