3-9. INTRODUCTION
In the OR, there are many hazards in addition to those of fires and explosions, which must be eliminated to ensure a safe area for patients and personnel. Constant alertness and care are the only means by which they can be removed. The common types of accidents because of hazards other than fire and explosion and the measures used to prevent them are discussed below.
3-10. UNCONSCIOUS OR SEDATED PATIENTS
Numerous hazards pose dangers to unconscious or sedated patients. The specialist must therefore be especially cautious when caring for such patients.
a. Attendance of the Patient. Never leave an unconscious or sedated patient alone on the operating table, stretcher, or in a wheelchair. He may fall or roll from the table and injure himself. A sedated patient may be confused or disoriented in addition to being drowsy and because of this, he may attempt to get off the table or stretcher and thereby injure himself. Ensure that side rails are raised and locked into position.
b. Transportation of the Patient. Exercise care when transporting the patient to and from the OR so that he is not injured going through doors and hallways. Restrain the patient lightly to prevent him from rolling from the stretcher during transportation. Ensure that side rails are raised and locked into position. Cover him adequately to avoid chilling.
c. Application of Restraints. Apply restraints so there is no pressure on the nerve, no impairment or respiration, and no obstruction of circulation.
d. Position of the Patient. Keep the body of the patient in proper alignment when placing him in position for surgery. There should not be unnecessary strain on the muscles. All braces and attachments used in positioning the patient must be padded. When the patient’s position is to be changed, he should be moved slowly and gently to prevent circulatory depression.
e. Removal of Prosthesis. All removable prosthesis will be left on the ward, properly identified and stored. A final check will be conducted in the OR to ensure that all prosthesis (false teeth, false eyes, and so forth) has been removed.
NOTE: The surgeon may wish to have a prosthetic device left in place for the performance of certain reconstructive surgery. In this event, he will write an order on the patient’s chart for the benefit of the nursing unit personnel. Also, the OR Schedule should include a notation to leave the prosthetic device in place.
3-11. TRANSPORTING THE PATIENT
a. Discussion. Within any treatment facility, the methods and procedures used for taking a patient into and out of an OR must be implemented in such a way that the patient is not harmed in the process. The methods and procedures in use vary, depending upon the type of medical installation. For example, at an aid station caring for the combat wounded, transporting the patient prepared for surgery may involve little more than lifting the litter onto litter supports and reversing the procedure after surgery.
In a large hospital, a more elaborate procedure is necessary. Regardless of the type of treatment facility, however, the basic purpose of transporting the patient is the same–to move the patient safely in and out of the OR. To this end, the OR specialist transporting patients should observe many precautions.
b. Responsibility of the Operating Room Specialist. In a large hospital, the circulator is often the person who transports the patient to the surgical suite. However, another specialist from the surgical staff may be assigned to transport the patient when the surgery load is heavy, when the distance from nursing unit to OR is long, or when local policy so prescribes. The anesthetist and surgeon always accompany the patient to his post-surgical destination. The specialist is responsible for the patient’s safety and well being whenever he is transporting the patient. Therefore, the specialist must know the appropriate procedure for obtaining and transporting the patient. The specialist must know how to recognize and deal with symptoms of distress in the patient and know the location of emergency supplies and equipment along the route. The specialist must never leave the patient unattended on transporting equipment. One person must be with such a patient at all times. In addition, the specialist must account for the patient.
c. Preliminary Preparation.
(1) Preparing the litter.. The specialist’s first step in transporting the patient is to “dress” the litter (see figure 3-1). This is to be done in such a way as to ensure the safety and comfort of the patient while in transit. The specialist does this procedure as follows:
(a) Place a sheet, folded in half, lengthwise, on the mattress of the litter and tuck it under the mattress all around.
(b) Open fully a second sheet, centered lengthwise, and place it in the litter with one edge at the head of the litter. Now fanfold the sheet from both sides and fold the remaining material at the foot of the mattress.
(c) Place a folded sheet on the litter for use as the cover. If the patient is likely to need additional covering during transport, provide a sufficient number of blankets, made of cotton only. Also place a safety strap, or straps as local policy may require, around the litter (see figure 3-1). Check the OR Schedule and write the patient’s name on a piece of paper for reference when on the nursing unit. The OR Supervisor or the OR NCOIC usually directs the specialist to transport the patient.
(2) Accounting for the patient.
(a) Just before leaving the surgical suite, the specialist should draw a circle around the patient’s nursing unit number on the OR schedule. This will indicate to other team members that the process for delivering the patient to the OR has been started.
(b) When he brings the patient into the OR, the specialist makes a diagonal mark across the circle.
(c) When the patient is taken from OR, the specialist makes another diagonal mark across the circle so that the final appearance of the nursing unit number is like this–42A. Thus, the patient is accounted for at all times. The particular method may vary, but each OR uses some system to save time and avoid confusion.
d. Identifying the Patient.
(1) Report to the charge nurse. Immediately upon arriving on the nursing unit, the specialist who is to transport the patient reports to the charge nurse, announces the name of the patient, and is told the location of the patient. The Specialist is given the patient’s chart, which should contain all laboratory reports, the signed operative permit, and the patient’s X-rays. He places these under the foot of the litter mattress.
(2) Specialist’s attitude and manner. The specialist must do his best to inspire confidence in the patient. All patients are usually fearful at this time of what may happen to them. Therefore, the specialist must be cordial, considerate, tactful, and accepting of the patient’s behavior. A pleasant greeting and explanation of what he is going to do will be appreciated by the patient. Avoid flippancy and apathy.
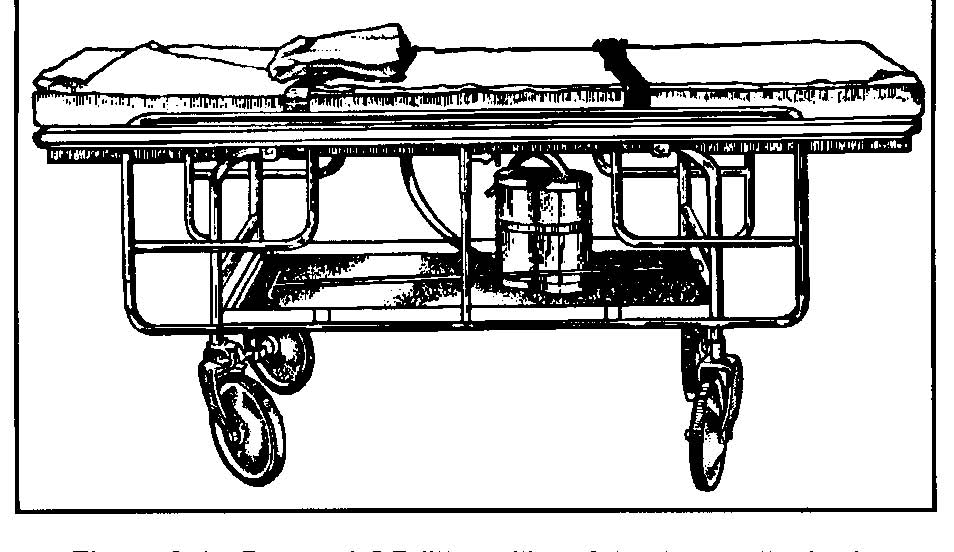
(3) Confirm identification. Having greeted the patient with a pleasant “good morning” and checked the patient’s bed card against the name he has written on the paper, the specialist asks the conscious patient–“What is your name?” (A sedated patient will often agree with any question, which requires only a yes or no answer.) The specialist also checks the hospital identification band (see figure 3-2) worn on the patient’s wrist. Local policy may require the charge nurse or someone else on the ward to confirm identity of the patient.
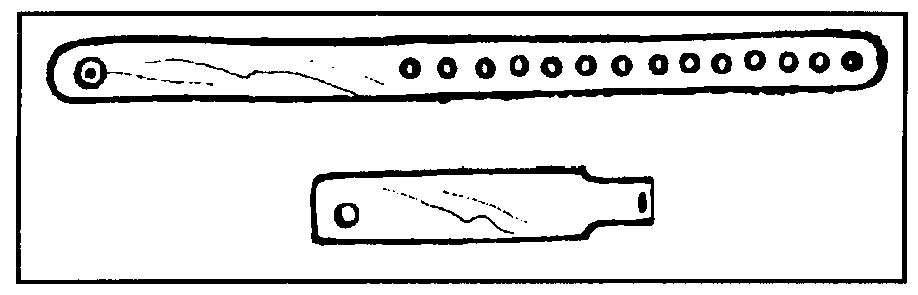
(4) Ensure that the patient’s preparation is complete. The patient scheduled for surgery is to be attired as prescribed by local policy. The specialist is to put an OR cap on the patient’s head in such a way as to cover his hair. Jewelry and prosthetic devices are to be removed by nursing unit personnel and put in a safe place to prevent loss and to protect the patient from possible hazards while he is unconscious. Exceptions may include a patient’s wedding ring and religious medal. The ring is to be taped securely to the patient’s finger. A religious medal, if the patient desires to wear it, is to be taped directly to the skin. The patient is never to wear such a medal, or any other item around his neck during surgery. An additional exception is a prosthetic device that the surgeon wishes to have left in place. The OR specialist should make a quick but thorough check to see that the patient is in readiness for transportation to the OR.
NOTE: Remember that the patient’s wedding ring and/or religious medal may be taped to his skin ONLY if these objects will NOT interfere with the surgical area. (See figure 3-3.) If this is the case, local policy will dictate the correct procedure to follow.
e. Transferring the Patient to the Litter.
(1) If the patient can help himself, the specialist should proceed as follows:
(a) Release the safety straps and cover the patient with the cover sheet from the litter.
(b) Pull the bedclothes to the foot of the bed, leaving the cover sheet over the patient.
(c) Unfold the fan folded litter sheet and move the litter parallel to and against the bed. Check to see that the wheels on the bed are locked.
(d) Stand on the free side of the litter, reach across it and keeping it steady, place your arms under the patient’s shoulders and thighs, and assist him in moving onto the litter. The patient should lie on his back with arms at his side.
(e) The previously fan folded sheet is brought up from the sides and foot to cover the patient completely. Cover the patient additionally if necessary and tuck the covers under the litter mattress. If necessary, use cotton blankets.
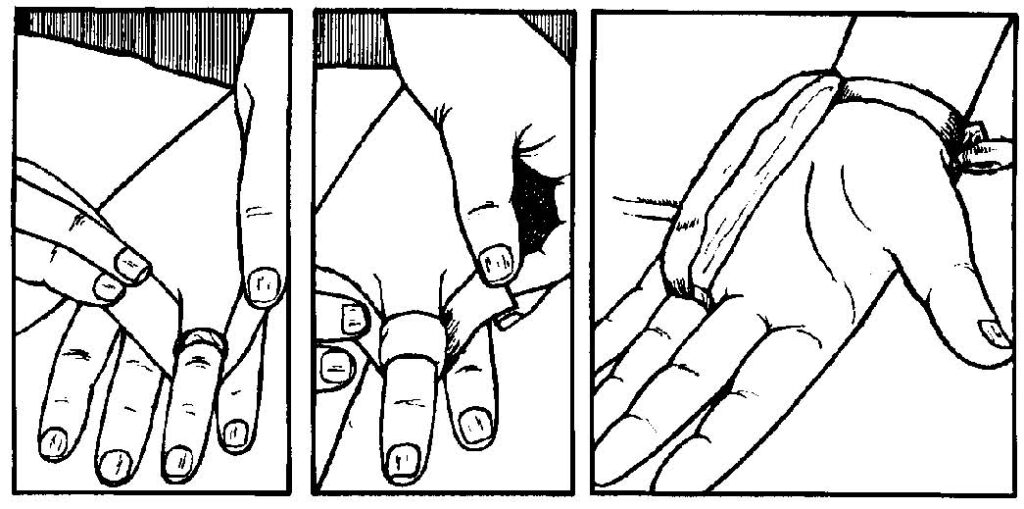
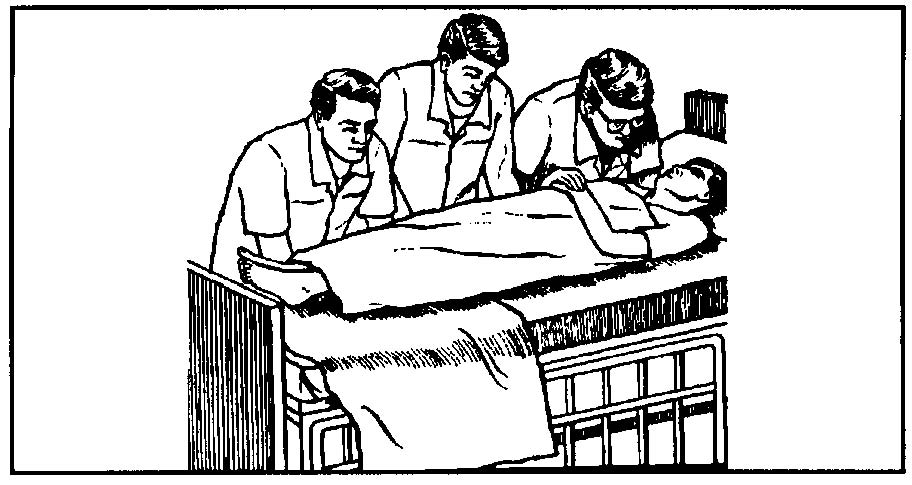
(f) Fasten the safety straps snugly over the patient’s thighs and the chest, and under and around the litter. Thus, both the patient and the specialist are assured that the patient will not fall off. Do not fasten the straps too tightly, as the patient’s circulation may be impaired. The straps should be secured in such a way as to enable the specialist to run his hand, palm down, between the strap and the patient (see figure 3-4).
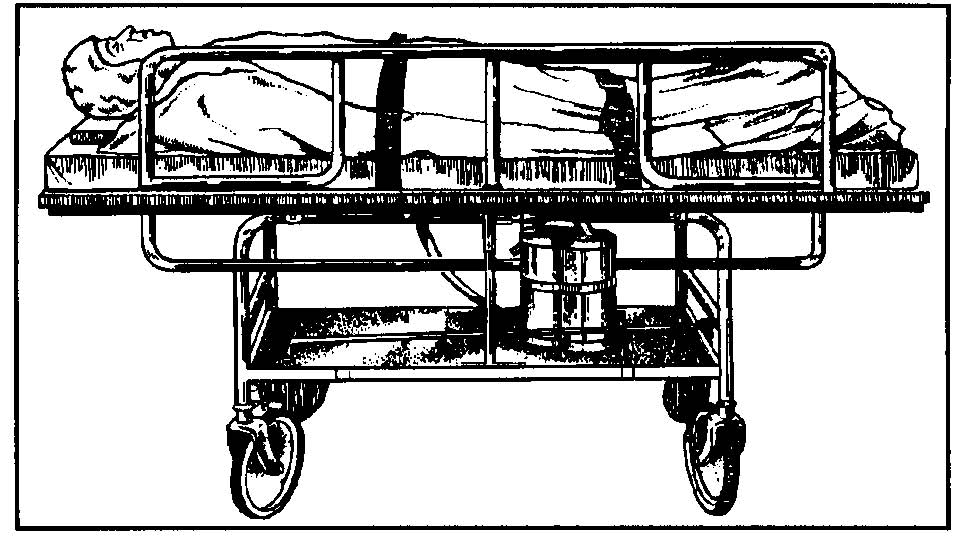
(Note position of side rail and safety straps.)
(g) Raise and lock litter side rails.
(2) If the patient cannot help himself, he must be lifted onto the litter. A team of at least three people is required to transfer an adult patient from the bed to the litter. They should proceed as follows:
(a) Release the safety straps, cover the patient with the cover sheet, and remove the bed clothing as in (1)(a) and (b) above.
(b) Place the litter at a right angle to the bed, with the head of the litter at the foot of the bed. Unfold the fan folded-litter sheet.
(c) Lock the litter wheels. Make sure that the bed wheels are also locked.
(d) Team member number one. Slide one hand under the patient’s head and to his opposite shoulder so that the patient’s head rests in the bend of the elbow. Place the other hand under the patient’s shoulders and his opposite arms (see figure 3-5A).
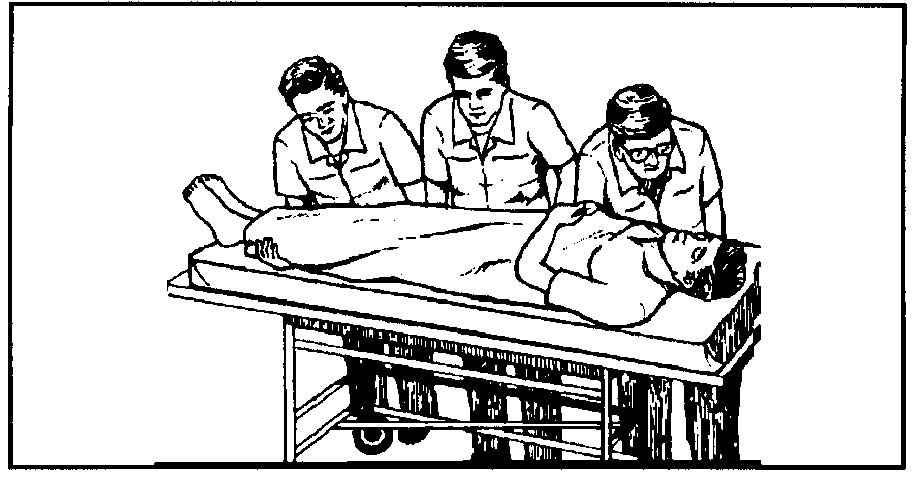
(e) Team member No. 2: Place both hands, palm up, under the patient’s hips. (See figure 3-5B).
(f) Team member No. 3: Place one hand under the patient’s thighs and the other under the calves of his legs.
(NOTE: Cover sheet omitted for visual clarification.)
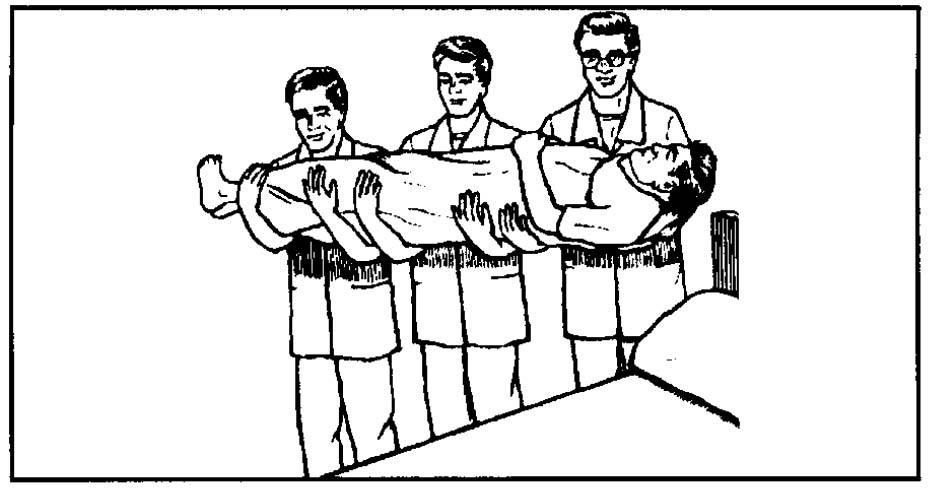
(g) On signal, draw the patient to the edge of the bed, tilt him slightly toward the team members’ chests, and lift him from the bed (see figure 3-5B).
(h) On signal, turn so that the patient’s head is toward the head end of the litter, advance to the litter, and carefully place the patient on the litter (see figure 3-5C).
(i) Cover the patient additionally if necessary and tuck the covers in as described above.
(j) Fasten the safety straps as described in (1)(f) above (see figure 3-4).
(k) Raise and lock side rails.
(3) Whenever the patient is connected to some kind of apparatus, the specialist should carry out additional safety measures as follows:
(a) If the patient has an IV running, the bottle should be suspended on a litter standard. The litter standard has a plate that, when slipped under the litter mattress will hold the standard upright and support the IV supply bottle. This should be placed near the middle of the litter (never at the head). Thus, if it should fall, it is less likely to injure the patient. The team members lifting a patient with an infusion running should exercise care so as not to disturb the setup. Protection is afforded by splinting the patient’s arm. A fourth person may be required to hold the infusion bottle while the patient is being transferred to the litter. If a fourth person is not available, the IV tubing must be clamped off and the bottle hung over the finger or the arm of one of the three people lifting the patient. The bottle is then hung on the standard and the clamp opened. If no litter standard is available, another person must accompany the specialist and the patient to the OR to hold the IV bottle at the same height above the patient as it was in the patient’s unit.
(b) The management of drainage equipment will vary with its type and function. If the patient has a urethral catheter connected to a tube leading into a drainage bag, the specialist should clamp the tube. Similar technique is to be used with suction tubing. Drainage will be restarted in the OR if the surgeon desires.
(c) If there is chest drainage, the tubing should be double-clamped on the nursing unit. An assistant should carry the drainage bottles at a level below the height of the patient’s chest.
f. Wheeling the Patient. One specialist can safely wheel the patient on a litter if the route to the OR is smooth and does not include steeply inclined ramps and if the patient has no special apparatus attached which requires the attention of an additional person. The specialist is to push the litter ahead of him, guiding it from the head end. He is to move at a safe pace, being careful not to bump anything or anyone, not to turn corners sharply or otherwise disturb or frighten the patient. When entering the elevator the patient is wheeled in headfirst. The specialist must not smoke while wheeling the patient.
g. Arrival at the Surgical Suite. Upon arrival at the surgical suite, the specialist should report to the anesthesia department and to the OR supervisor or the NCOIC; in addition, as stated above, he should draw a diagonal mark across the patient’s nursing unit number on the OR schedule. The specialist remains with the patient (unless he is properly relieved) until the patient is to be transferred onto the operating table. The specialist is then to assist in transferring the patient to the table.
h. Care of the Patient Awaiting Surgery. The patient may be brought to the surgical suite before the scheduled time for his operation, necessitating a wait somewhere outside the OR in which his surgery will be performed. It is important that the patient remains relaxed and comfortable during his wait, since a favorable environment at this time contributes much to a smoothly conducted, successful operation. Therefore, the OR specialist should place the patient’s litter away from glaring overhead lights, into a dimly lit area.
The specialist, as well as all of the personnel in the surgical suite, should cooperate in maintaining a quiet atmosphere, because the patient is especially sensitive to noise at this time. Loud talking, laughing, discussion of operative procedures within his hearing, or other inappropriate behavior can frighten the patient and destroy his confidence in the surgical team. In addition to making the patient’s environment as calm and serene as possible, the specialist may make the patient more comfortable by placing a pillow under his head and by allowing him to turn on his side; however, first the specialist must ensure that these measures are not contraindicated (made inadvisable).
i. Transferring the Patient to the Operating Table. The patient may be transferred to the table either inside or outside the OR. In either case, the sheet coverings on the patient are loosened while the patient is outside the OR in order to hold to a minimum the fanning of the covers, with their microbial population, in the OR. The patient is transferred with the cover sheet over him.
(1) Outside the operating room. When the patient is transferred outside the OR, the operating table is brought out to the litter. After the patient is transferred, the table is wheeled back into the OR and the wheels of the table are locked.
(2) Inside the operating room. When the patient is placed on the table inside the OR, the litter is wheeled into the OR and placed alongside the table. After the patient is transferred, the litter is wheeled from the room.
j. Procedure During and After Surgery.
(1) Preparation of the litter. As soon as a patient has been transferred from the litter to the operating table and while the patient is still in the OR, the litter is to be stripped, cleaned as necessary, and “dressed” to await further use. These procedures may be carried out by the circulating specialist or by another person assigned by the OR Supervisor or NCOIC. The person who dresses the litter should also see that hand towels and an emesis basin are at hand to accompany the patient to his post-operative destination. Some postoperative patients become nauseated and vomit during transit. The emesis basin and towels are used to keep the patient clean and comfortable.
(2) Delivery of the patient. Upon the completion of surgery, the patient is lifted onto the litter and positioned. The safety straps are fastened, and he is transported to either the recovery room or the nursing unit. Both his position and his destination depend upon the type of anesthetic and the kind of surgery the patient has undergone.
(a) The patient who has been given a general anesthetic should be placed in a lateral recumbent (side-lying) position unless this position is contraindicated by the surgery performed. In which case the patient should be placed either supine (on his back) or prone (on his abdomen), with his head turned to one side. Turning the head to one side facilitates the normal drainage of secretions and helps prevent the aspiration of secretions and vomitus. The endotracheal tube, if one has been inserted, should be left in place and kept free from obstruction until the patient’s gag reflex returns. Usually, the anesthesiologist or anesthetist accompanies the patient to the recovery room, and there is assisted by either the circulator or the specialist who assisted with anesthesia during surgery. The patient who has had a spinal anesthetic should be transported to the recovery room in either a dorsal recumbent (supine) position or prone position.
(b) When brought into the recovery room, the patient may be transferred to recovery room equipment or remain on the wheeled litter for care by recovery personnel. (In either case, the specialist should put side rails in place to ensure that the patient will not fall off the bed.) A patient expected to remain in the recovery room for only a short time may afterwards be wheeled to the nursing unit on the same litter on which he was brought to the recovery room. If a lengthy stay in the recovery room is anticipated, the patient is often placed in a recovery room bed immediately after surgery. An arrangement that provides for a minimum number of transfers of the postoperative patient protects the patient who has had spinal or general anesthesia from sudden and dangerous drops in blood pressure.
(c) The trip for the delivery of the patient to the nursing unit may originate in the OR or the recovery room. A patient who has given a local anesthetic or regional block is transported directly from the OR to the nursing unit by an OR specialist. If the distance from the OR to the nursing unit is short, one OR specialist may transport the patient. However, two persons may be assigned when the trip is time-consuming because of either the distance or other factors.
(d) While transporting a patient, the specialist must be continually observant for symptoms of respiratory difficulty, shock, or hemorrhage, and should be ready to employ emergency techniques that are within his capability. He must know the location of emergency equipment such as suction machines and oxygen therapy equipment along the route. He must also be able to summon professional aid and assist with emergency procedures instituted by the MC Officer or the AN Officer who responds to his call for help. Upon arriving on the nursing unit, the specialist is to report to the nursing unit office, return the patient’s chart, and request help as needed for transferring the patient onto his bed. The specialist and any designated helpers then wheel the patient to his bed and place him upon it.
k. Other Means of Transporting the Surgical Patient. All pieces of equipment brought from the nursing unit must be damp-dusted with alcohol or as directed before being brought into the OR. This includes the beds, turning frames, and equipment for transporting infants discussed below.
(1) Adjustable (Gatch) bed. The patient may be wheeled to the OR upon his bed. A patient who is seriously ill or one who is to have cardiac or chest surgery is in this way spared the procedure of being transferred to a litter, a procedure that may endanger the life of such a patient. The bed is adjusted to place the patient in the position that is most healthful and comfortable to him. At least two specialists are required to wheel the patient in bed to his destination. The specialists must secure side rails onto the bed and be very careful not to traumatize the patient, either physically or mentally, during transit.
(2) Fracture bed. The surgeon may order that a patient scheduled for orthopedic surgery be transported in his fracture bed. This means of transportation is especially desirable when traction has been applied preoperatively since removing it could put the body out of alignment. At least two specialists are required for transporting a patient in a fracture bed. The specialists must use every precaution during transit to avoid disturbing the traction or otherwise injuring the patient.
(3) Turning frame or reversible bed. Surgeons often order that patients upon Stryker frames or Foster beds be transported on them. The specialist must apply several safety straps before transporting the patient since patients on turning frames are often helpless (because of injuries to the spinal cord or the brain, certain kinds of orthopedic conditions, severe burns, paralysis, or the application of traction). At least two specialists must be available for transporting the patient, and they must take the utmost care to avoid traumatizing the patient.
l. Special Means Used for Infants and Children.
(1) The specialist may be required to wheel a small child or an infant in a pediatric crib or a bassinet. When using either of these methods, two specialists may be required, as cribs and bassinets are quite awkward to handle.
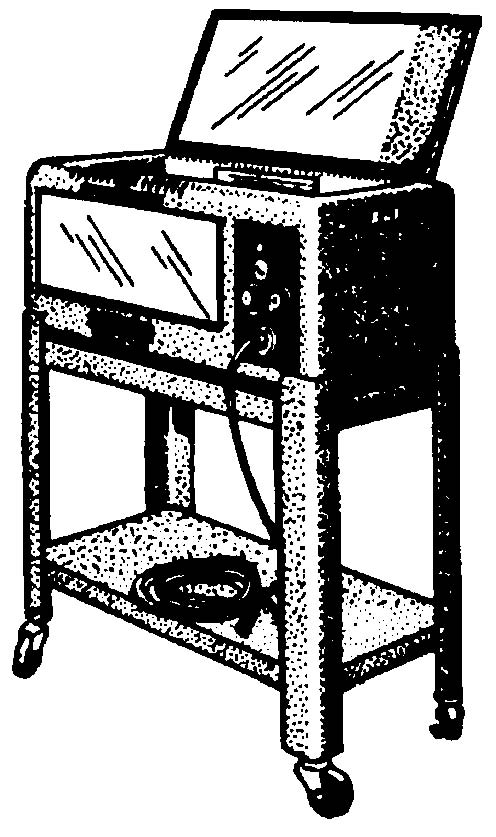
(2) Tiny infants may be brought to the OR in an incubator. An incubator (see figure 3-6) is a small crib unit equipped with an inlet for oxygen, a mechanism for supplying heat, and a temperature-regulating mechanism. The incubator is mounted on a wheeled stand. Oxygen may be supplied by means of either a small cylinder or a large cylinder and is piped into the incubator through a tube. If the oxygen is to be kept running during transport, the specialist must check the liter flow gauge both before and during transit.
3-12. THE IDENTIFICATION AND USE OF DRUGS
a. Discussion. The improper identification, administration, or use of drugs may endanger the life of a patient. This improper handling of drugs includes such hazards as giving a patient a wrong drug, giving an inaccurate dosage of the right drug, and failing to take appropriate precautions when extremely dangerous drugs (such as phenol and cocaine) are to be used. The specialist may avoid such errors by following the safety rules set forth below.
b. Reading the Label. The specialist preparing the drug should read the label on the vial, ampoule, or bottle three times–when taking the drug from its storage place, when ready to pour or withdraw the drug, and just before either discarding the drug container or returning it to its storage place. If the drug is handed to another person (such as the scrub or doctor), then that person should be shown the label also. The specialist is never to use a drug that has changed color or one from an unmarked or poorly labeled container.
c. Pouring the Excessive Amount of Drug. If the specialist pours or withdraws an excessive amount of a drug, he is to discard the excess drug. He is not to return it to the supply container.
d. Drugs for Use Within the Operative Area. The label of a drug prepared for use within the operative area is to be checked by two persons. In addition, the specialist states the name of the drug when handing it to the surgeon.
e. Use of Cocaine. Cocaine must be kept in a locked place and must be accounted for, since it is classed as a narcotic agent. Cocaine is a highly toxic drug, and therefore, the following precautions should be observed in its use.
(1) Cocaine solution should be stored in a dark bottle away from light and never for duration longer than 2 weeks. The length of storage time will depend upon the surgeon. Many medical officers prefer a freshly made solution each time it is used for topical anesthesia.
(2) Cocaine is never to be injected. It is used for topical anesthesia only.
(3) Dosage should be checked carefully. Cocaine is supplied in ampoules containing either 3.5 g or 0.5 g of the drug and is usually used in solutions of two, four, and ten percent.
(4) Personnel who prepare cocaine solution for use on a patient must be especially careful to ensure that they make no error in the identification of this drug. To assist with the accurate identification of the drug, pharmacy personnel may place a coloring agent into cocaine solution.
3-13. ADMINISTRATION OF BLOOD
Certain safety precautions must be observed when administering blood to a patient to help prevent errors and reactions. The circulating specialist usually assists with the administration of blood.
a. Unless ordered otherwise, the blood is to be kept refrigerated until it is to be administered.
b. The information recorded on the label on the blood container is to be checked against the Standard Form 518, “Medical Record–Blood or Blood Component Transfusion,” to be sure the blood is that which is intended for the patient. The container and SF 518 should be checked by a medical officer (usually the anesthesiologist) as well as the circulating specialist before the transfusion is started.
c. Unfiltered blood is never to be given. A blood recipient set, which is equipped with a filter is to be used.
d. The unit of blood is to be rotated gently to disperse the cells evenly. The blood is not to be shaken, as this would damage the red cells.
e. When pressure is being applied to a container of blood to speed the rate of transfusion, the container must be kept under constant observation. As soon as the container has less than a quarter of its total contents remaining, the pressure must be released. These precautions are taken to prevent the occurrence of air embolism, which could prove fatal to the patient.
3-14. SPONGE COUNT
a. Discussion. In order to account for all sponges, thus ensuring that none have been accidentally left in the patient, a sponge count is taken at least three times:
(1) By the personnel who wrap sponges or place them in a surgical pack for sterilization.
(2) By the circulator, scrub, and registered nurse (RN) immediately before surgery begins. The circulator then records the sponge count.
(3) By the circulator, the scrub, and RN, and again when the surgeon begins the skin closure. A sponge count may be taken three times during an operation, as in a cesarean section when the sponge count is made before the uterus is closed and again before the abdominal incision is closed, and again as the surgeon is closing the skin. A registered nurse always witnesses the count of sponges in the OR.
b. Repeating the Count. There should be no interruptions while the sponge count is being made. If there is any doubt about the count, it must be repeated.
c. Measures Taken During Surgery. During surgery, loss of sponges may be prevented by various methods. Measures to be taken by the scrub and the circulator include those listed in ((1)-(2), below). Additional measures may be used depending upon local policy or the preference of the surgeon.
(1) Sponges used for the patient’s skin preparation are not radiopaque. The circulator is to remove those sponges from the immediate operative area and to secure them in a conductive bag.
(2) Place stick sponges on sponge forceps for use within a cavity; place Kitner sponges on curved (Kelly) forceps.
3-15. NEEDLE AND INSTRUMENT COUNTS
a. Accounting for Needles. The scrub and the surgeon should work cooperatively to make sure that no needle is left in the patient:
(1) Needle counts should be done on a one-for-one basis to the surgeon; that is, the scrub should receive the needle the surgeon has just used before handing him another one. If a needle is broken, both parts must be given to the scrub.
(2) At NO time should there be a free needle (one not on a needle holder) on the Mayo stand or within the operative field.
(3) The scrub should know the number of needles in actual use.
b. Accounting for Instruments. Instrument counts are seldom necessary, unless it is common practice to count them in the state where the Army hospital is located or on cases in which instruments might easily be lost.
3-16. CARE OF TISSUE SPECIMENS AND FOREIGN BODIES
a. Handling of Specimens. A specimen is anything surgically removed from the patient. It may include bone, soft tissue, or foreign body. The improper handling of specimens may result in a mistaken diagnosis, a delay in treatment, or a second operative procedure, any of which may jeopardize the life of a patient. The circulator is responsible for the proper handling of the specimen. He should take the following measures:
(1) Label the specimen container properly, in accordance with local policy. The circulator must identify the specimen on all the proper forms. A gummed label is usually completed and placed on the specimen container. In addition, Standard Form 515, “Medical Record–Tissue Examination,” should be filled out in duplicate.
(2) Place the specimen in the appropriate container with the appropriate solution, usually a ten percent formaldehyde solution for routine specimens. However, the solution to be used is prescribed by the pathologist.
(3) Give special handling to those specimens requiring it. Always ask the OR nurse or the surgeon before placing a specimen in the routine solution. Examples of situations in which specimens may require special handling are as follows:
(a) Some specimens cannot go into the ten percent formaldehyde solution right away. Tissue for frozen section is one example. It is a specimen prepared for immediate diagnosis by quick-freezing, cutting a cell-thick layer, and viewing under the microscope. When the surgeon requests a frozen section which is usually indicated on the OR schedule, the specialist must be sure that the pathologists has been notified in advance, since the patient is on the OR table under anesthesia while the surgeon waits to hear if the tissue is malignant or benign. There cannot be undue delay! This specimen is placed in a moist towel or a Petri dish, never a sponge, by the scrub and handed to the circulator. He will give it to the designated person, probably someone from the laboratory. It is recorded immediately in the specimen log and signed for upon delivery. It must be delivered immediately to the pathologist. His results will be reported directly to the medical officer or nurse.
(b) Specimens of tissue to be examined for tuberculosis organisms are to be placed in saline solution. In addition, other specimens may be taken to the laboratory in saline solution when the surgeon wants the specimen examined immediately.
(c) When the specimen is a pap (Papanicolaou) smear (done in certain operative procedures to determine the presence of cancerous cells without having to excise tissue), glass slides with secretion from the suspected area are placed in solution of equal parts of ether and dehydrated alcohol (absolute alcohol).
(d) Specimens to be photographed are to be placed in saline solution or covered with a towel moistened with saline because formaldehyde solution discolors tissue.
(e) Some specimens are handled using sterile technique to avoid the possibility of introducing new bacteria. The pathologist’s report and in turn the medical officer’s diagnosis may be affected if sterile technique was not observed by all personnel when handling the specimen and foreign bacteria were allowed to contaminate it. Cultures are examples of specimens handled using sterile technique. A sterile member of the OR team uses two cotton tip applicators to swab the pus or fluid. When the material has been swabbed for culture, it is passed off to the circulator and should be placed in a culture tube and delivered to the laboratory as soon after being taken as possible.
b. Disposition of Foreign Bodies. Foreign bodies removed from a patient should be cared for according to local hospital policy. Such items may have legal significance outside the hospital; for example, police may desire a bullet that has been removed. The giving over of a foreign body to other than the appropriate hospital personnel is done only by the responsible medical officer.
3-17. STERILITY OF MATERIALS
To protect the patient from infection that could prove fatal, measures must be taken to assure the sterility of the materials used. Numerous measures are employed during the operation to maintain sterile conditions. The OR specialist has many duties in the employment of these measures that include the following:
a. Goods are to be cleaned, wrapped, and loaded in the autoclave (steam pressure sterilizer) in such a way as to facilitate their penetration by steam.
b. Goods are to be processed in the sterilizer at the temperature and for a period appropriate for the item or class of goods and the size of the packages being sterilized.
c. Sterilization indicators are to be placed inside the packs as a check on the sterility of the goods processed. These indicators consist of chemically treated, heat-sensitive paper. If the indicator fails to change color, the specialist will know that the temperature necessary for the sterilization of goods has not been reached inside the autoclave and thus he is to discard the pack as unsterile. If the indicator has changed color, the specialist is to consider the pack safe for use, even though the color change does not provide assurance that the temperature of 250ºF has been maintained long enough for steam to penetrate the depth of the pack. The specialist should be aware of the limitations of sterilization indicators while at the same time realizing their usefulness as a check on the sterility of goods. The method described in g below is used in order to gain absolute assurance of the sterility of autoclave goods.
d. Pressure-sensitive tape is used for sealing and labeling surgical pack wrappers and other items to be processed in the steam pressure autoclave. The paper tape backing changes color when subjected to steam sterilization, giving definite indication that the item has been autoclaved.
e. Upon their removal from the autoclave, packs are to be placed on a perforated surface until they have cooled. This precaution is observed because a condensation of moisture occurs underneath a hot pack when it is placed on a solid metal surface. The pack will absorb this water, thus contaminating the pack since the metal surface is not sterile.
f. The packs are to be dated immediately after they have been processed in the autoclave. This measure prevents confusion as to which packs have been autoclaved.
g. Periodic tests are run to determine whether or whether not autoclaves are actually sterilizing the goods being processed. These tests should be conducted weekly, and in some installations they may be carried out more often. The test is done by placing a bacterial spore test strip (a standard item) inside a large pack. After the pack has been autoclaved, the test strip is removed under sterile conditions, replaced in its packet, and sent to the laboratory. If no growth of organisms occurs within the designated period, the autoclave is sterilizing the goods. If a growth of organisms does occur, the autoclave in which the test strip was processed is not used until it is checked and repaired by maintenance personnel; and the items “sterilized” in that autoclave during the test period are considered unsterile and must be reprocessed and resterilized.
h. All measures necessary for the maintenance of aseptic technique are carried out while an OR is being prepared for an operation and during surgery.
3-18. ACCIDENTS TO OPERATING ROOM PERSONNEL
Serious injury to OR personnel may be prevented if each individual observes the following precautions:
a. Keep the floors free from spilled solutions to prevent falls.
b. Use padding when handling objects that are very hot in order to prevent burns.
c. Use the necessary precautions when handling electrical equipment to prevent shock.
d. Keep your body in proper alignment when moving patients and equipment to avoid back strain and muscle strain.
e. Use adequate support when it is necessary to reach high places. Do not stand upon chairs, fragile boxes, or other items that are not safe for such use.