1-11. INTRODUCTION
a. Discussion. The types of equipment and its arrangement will vary in different installations according to individual needs and preferences. Adequate but not excessive equipment should be available and arranged so that maximum efficiency is obtained with minimum effort. Modern OR equipment with but few exceptions is made of unpainted, durable, and easily cleaned corrosion-resistant metal (CRM). In addition, most of the items are equipped with casters to enable them to be moved quietly and with the least possible effort. The casters are made of conductive material–either metal or conductive rubber–for the same reason that floors are conductive (refer to paragraph 1-7b).
b. Illustrations. Many of the figures in this lesson show equipment used in Army hospital ORs. Equipment for use in the field is similar to that shown, except that bulky items for field use are characteristically constructed to permit knockdown (refer to paragraph 1-3b). The equipment shown in this lesson is that which is typically used during surgery. This type of equipment is considered standard items and is listed in the Federal Supply Catalog. A cardioscope, which is not shown, is used only for special kinds of surgery and will be purchased through normal channels. Any item not listed in the Federal Supply Catalog is nonstandard, if needed, and must be obtained through a local purchase request.
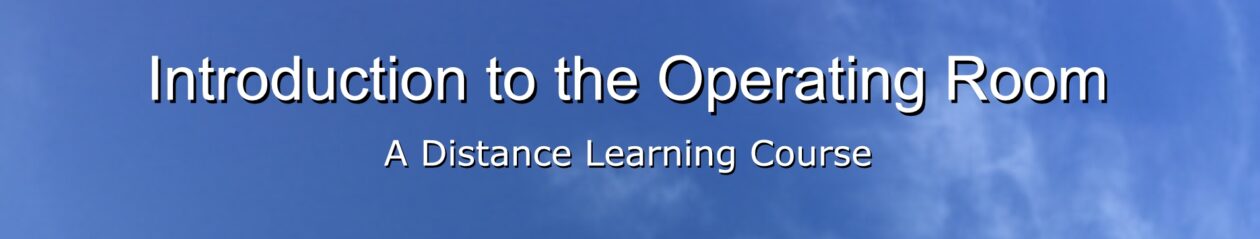
1-12. OPERATING TABLE
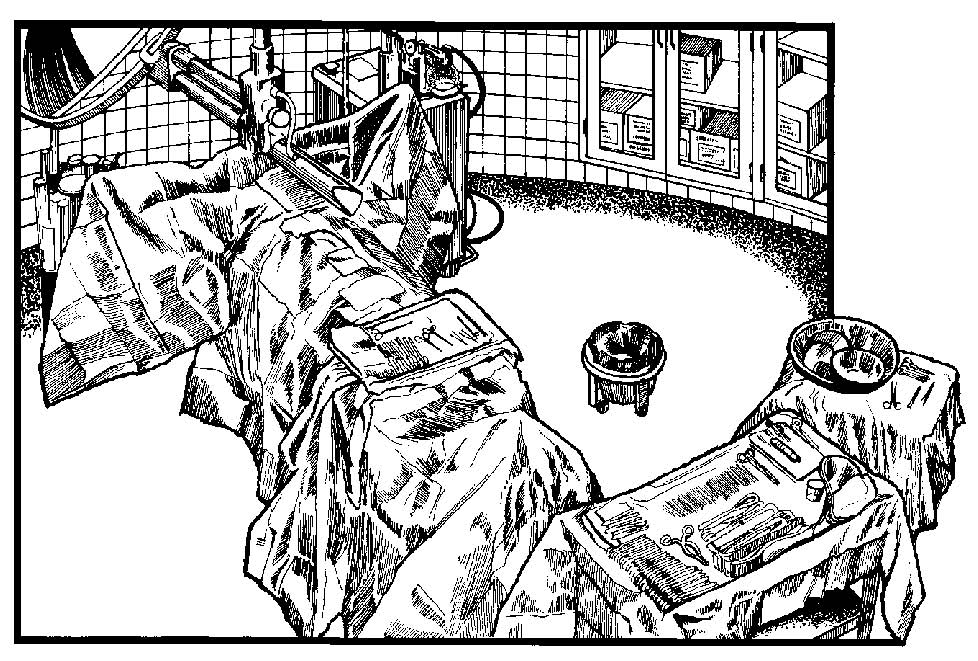
There are several types of operating tables (see figure 1-7) in use and all are rather complicated in construction and manipulation. They are designed so that they can be adjusted to the needs of the surgeon for any type of operation he may perform. The table is equipped with a hydraulic system. It is mounted on casters that are locked in place during surgery. The operating table shown in figure 1-7 is “dressed” or made up with sheets ready to receive a patient.
The enlisted 0R specialist assigned to circulate for an operation is responsible for assisting with the positioning of the patient. Therefore, he must have a detailed knowledge of the table as well as the many positions of the patient for surgery. A full discussion of the operating table, attachments, and use are set forth in Subcourse MD0927, Special Surgical Procedures I.
1-13. SURGICAL INSTRUMENT TABLES
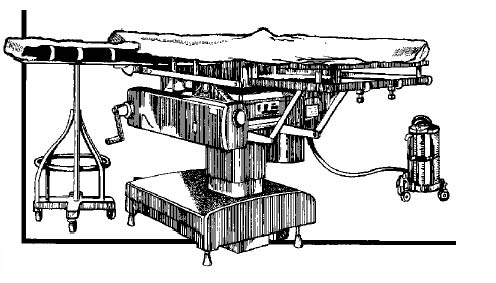
a. Mayo Stand. See figures 1-8, 1-11, and 1-12. This stand or table is small, and its height is adjustable. It is designed to overhang the operating table and hold instruments and other sterile items for immediate use and within easy reach of the scrub. The tray upon which the sterile goods are placed is detachable so that is may be sterilized for use during an operation.
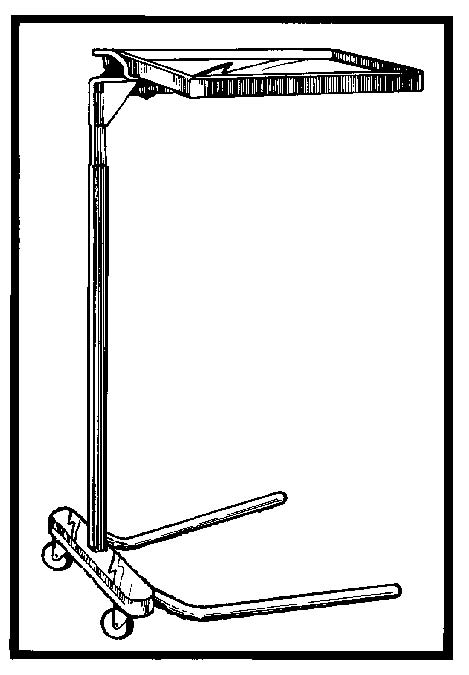
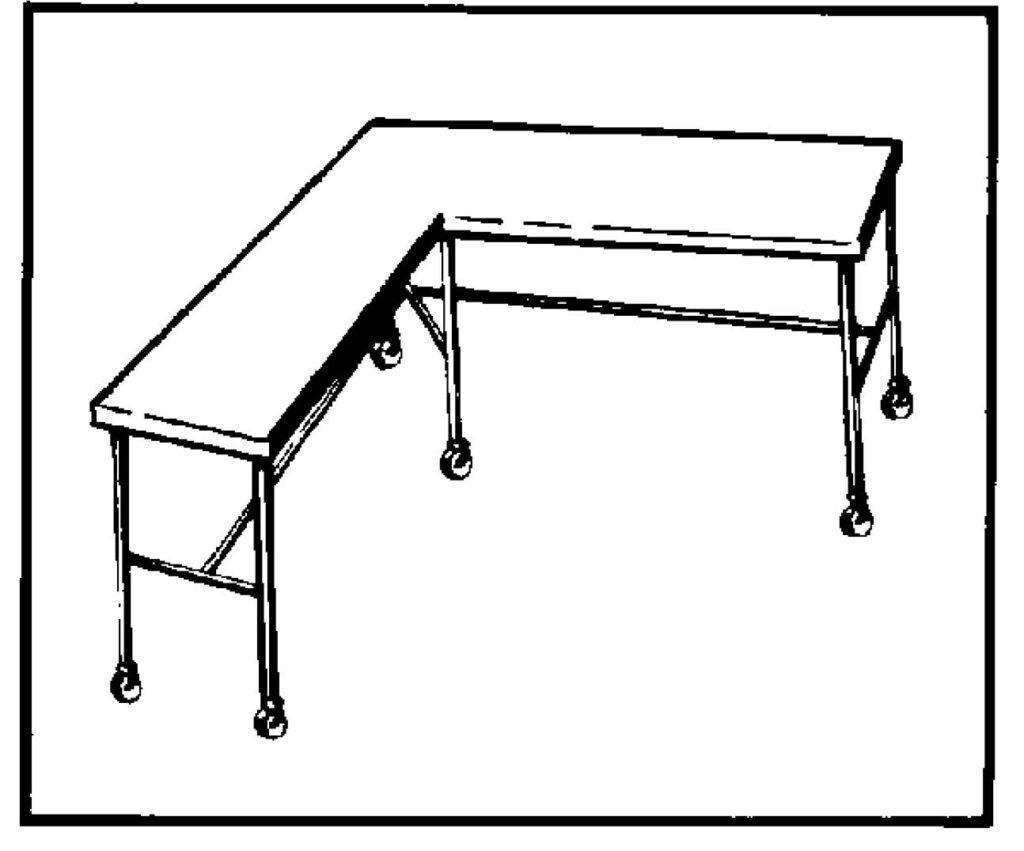
b. Large Tables for Instruments. See figures 1-9, 1-10, 1-11, 1-12, and 1-13). The largest table for instruments used in the OR is the angular or “L”- shaped table. The table provides an area where additional sterile supplies for the case can be arranged and stored until needed. If the number of supplies to be used does not require the use of the angular table, a smaller rectangular table is used. Both the angular table and the smaller rectangular table are often referred to as “back” tables. The “back” table is placed within easy reach of the scrub and is draped with sterile drapes for use during an operation. (See Figure 1-10.) There is also an undraped angular instrument table (back table).
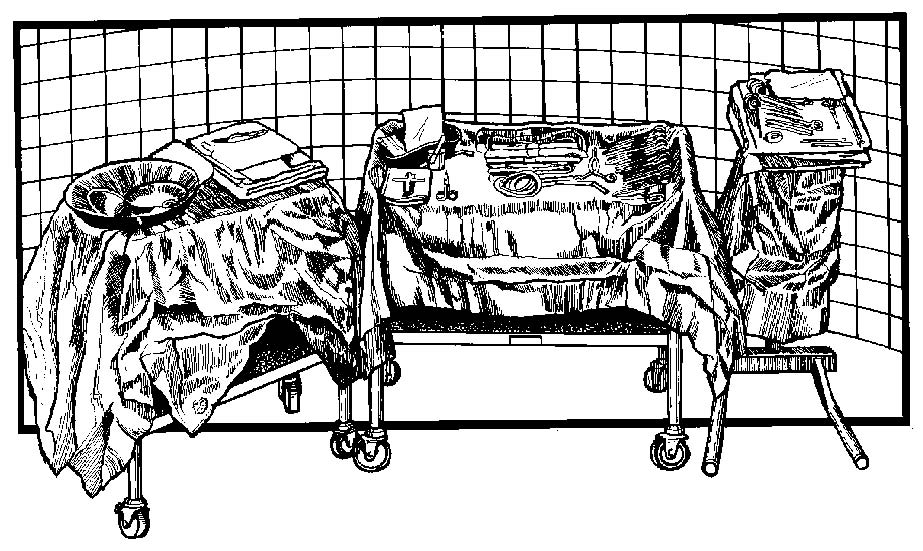
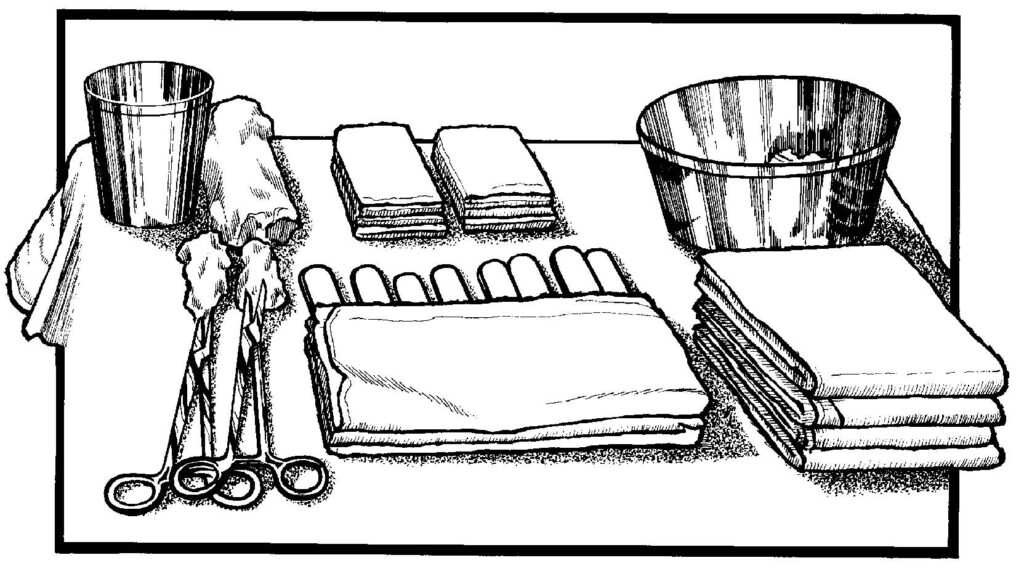
c. Table for Skin Preparation (“Prep”) Setup. Some type of a small instrument table is necessary for setting up a sterile field containing the materials needed to cleanse or prep the patient’s skin for surgery. Refer to figure 1-13.
d. Additional Tables. Depending upon the type of surgery to be performed, shelved instrument tables or small accessory tables may be needed in an OR in addition to those described in the previous paragraphs. For example, in ORs without recessed wall cabinets or in those with inadequate wall cabinet space, a small instrument table with shelves is used to hold the sutures, solutions, and medications that may be required during an operation.
1-14. ANESTHETIST’S EQUIPMENT
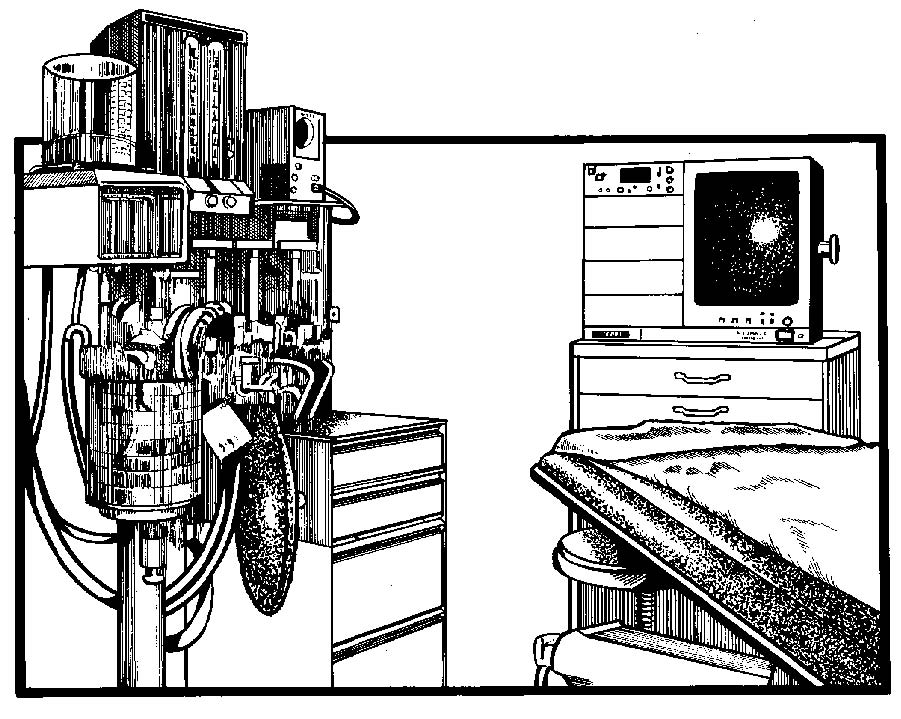
The anesthetist’s equipment is grouped together in the setting in figure 1-14.
a. Discussion. The items of equipment discussed below are cleaned and maintained by Anesthesiology Services personnel.
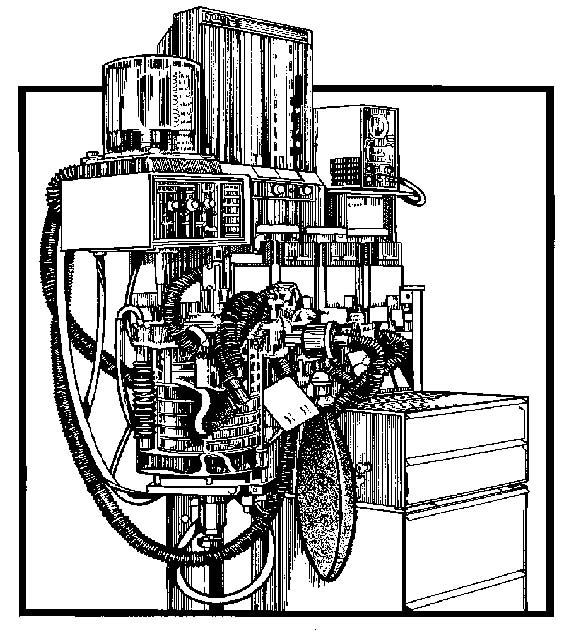
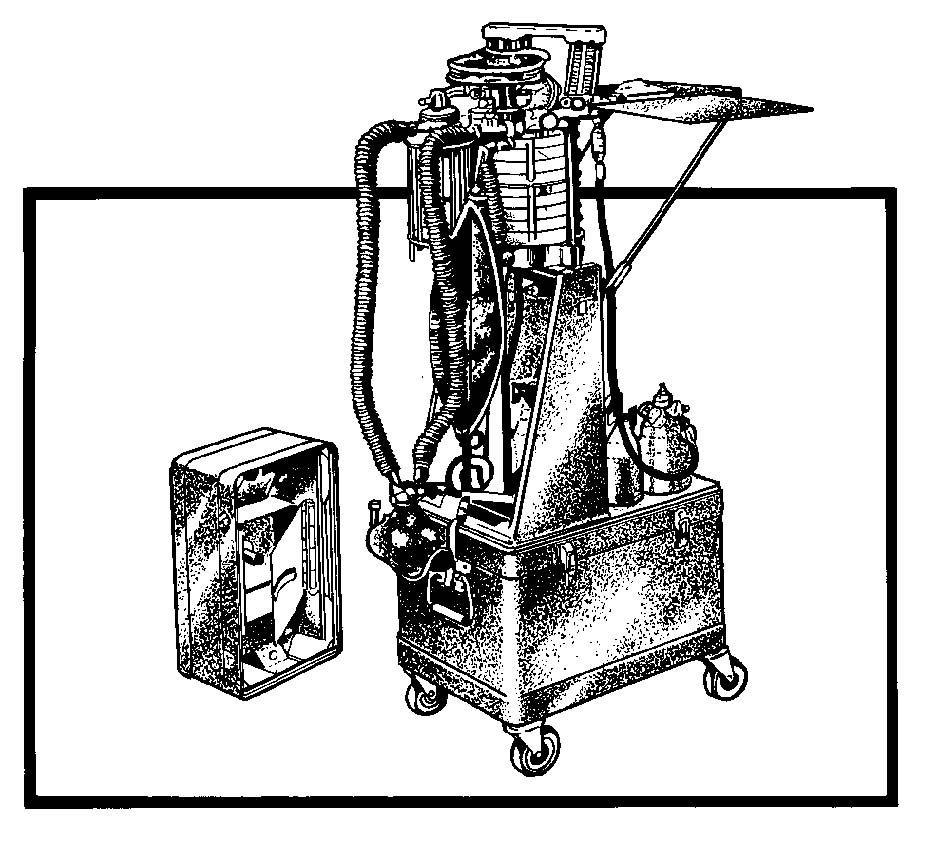
b.Gas Anesthesia Apparatus. (See figures 1-15 and 1-16). This is a mobile piece of equipment constructed to hold the following anesthetic materials.
(1) Pressure regulators for both oxygen and nitrous oxide.
(2) Inhaler tubes.
(3) Oronasal mask.
(4) Rebreathing bag.
(5) Water manometer (indicates the rate of flow of gases).
(6) Carbon dioxide absorber unit.
(7) Tanks of oxygen and nitrous oxide.
c. Table. The anesthetist’s table is small and low and is used to hold all of the additional equipment necessary for the administration of anesthesia. See figure 1-16, Anesthesia machine (field type).
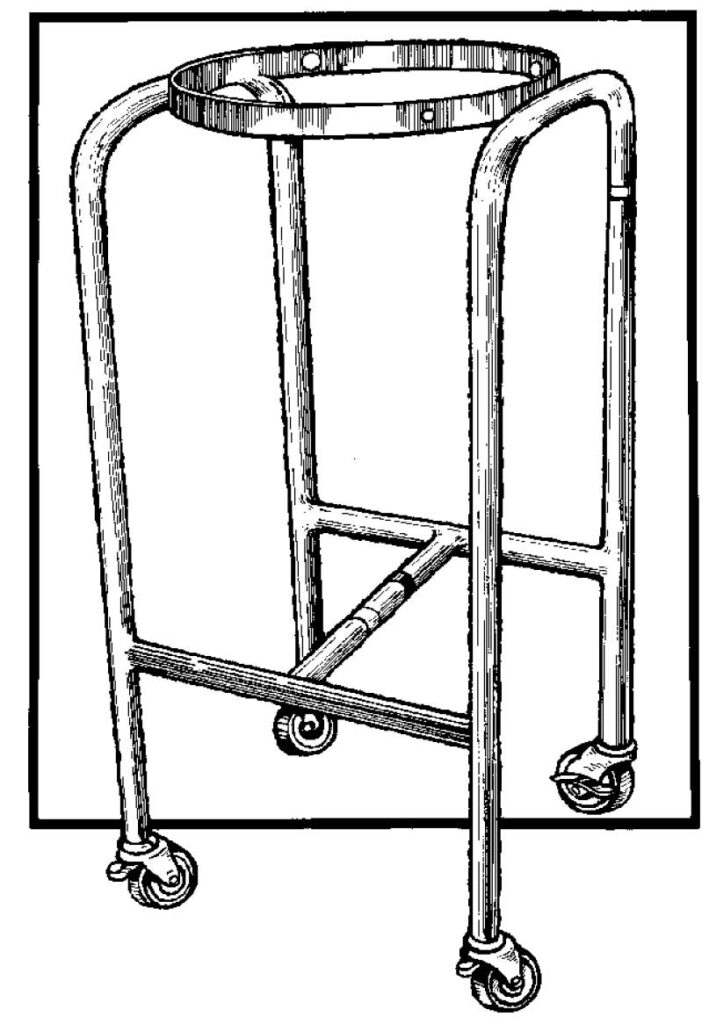
1-15. BASIN (RINGED) STANDS
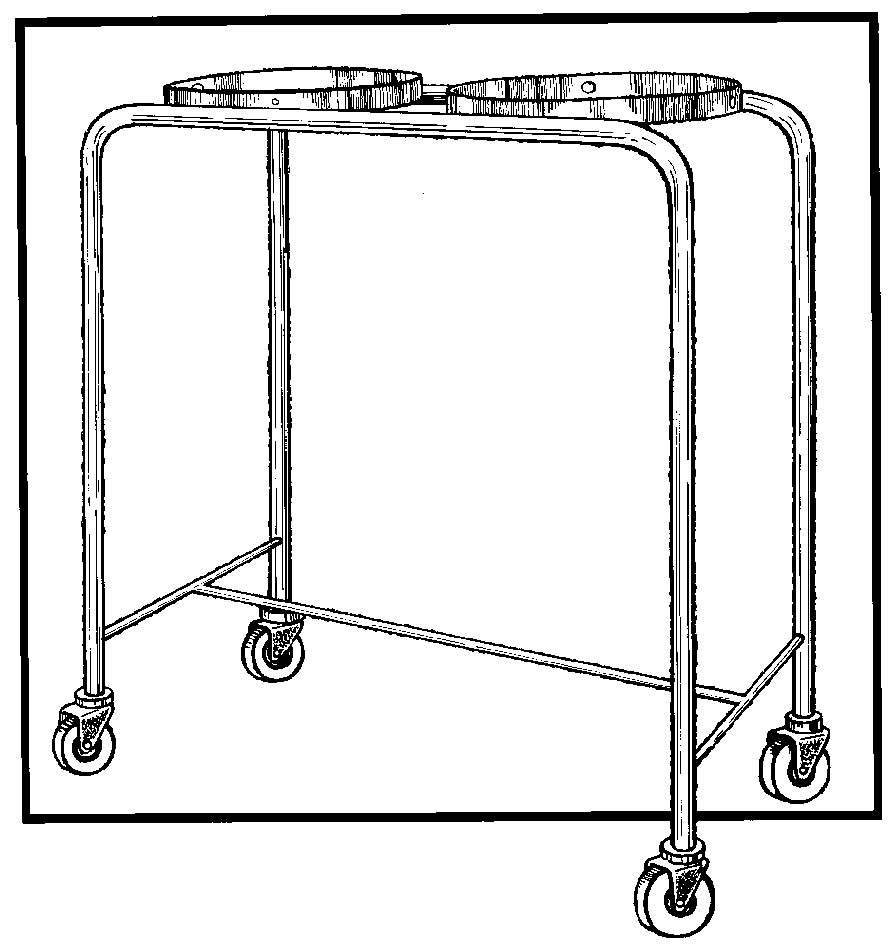
Double- and single-ring stands (see figures 1-17 and 1-18) are designed to hold basins of sterile solutions used during the operative procedure. A single-ring stand may be used to open instruments sets, and so forth. A double-ring stand is placed near the scrub who uses one basin for rinsing instruments, and so forth, the other for moistening sponges. Basin stands are equipped with casters to allow them to be moved easily.
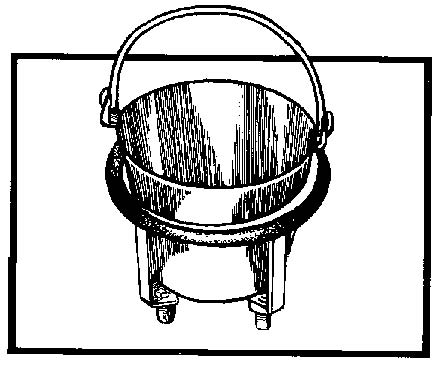
1-16. KICK BUCKETS
A kick bucket (see figure 1-19) is a large pail placed in a carriage with wheels. A kick bucket is put on each side of the operating table to serve as a waste receptacle. Kick buckets are convenient to use, easy to clean, and are easily movable with the foot. For surgery, kick buckets should be lined with a nonstatic-producing plastic liner to receive soiled sponges and waste material; thus, gross soil is kept off the buckets.
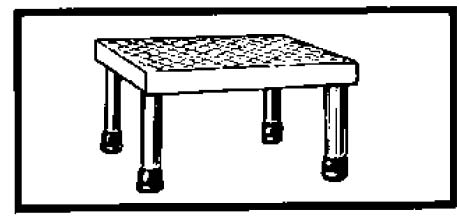
1-17. STOOLS
a. Revolving Stools. A revolving stool (refer to figure 1-14) is furnished for the anesthetist, who works in a sitting position. Another is provided for the surgeon if he is to sit during the operation, as he often does for vaginal and rectal operations. Note that the legs of the stool are equipped with rubber tips, assuring that the stool will remain where placed while a team member is sitting on it. These tips are made of conductive rubber.
b. Straight Stool (Footstool). See figure 1-20. These are small footstools, eight inches in height, constructed of metal with a rubber-covered top that may be used to increase the height of a team member. Note that these stools also have rubber-tipped (conductive rubber) legs to prevent them from moving while team members stand on them.
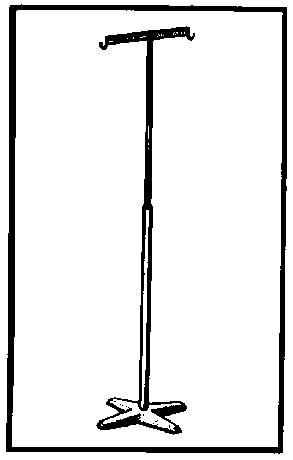
1-18. INFUSION AND IRRIGATOR STAND (INTRAVENOUSLY INFUSION STAND)
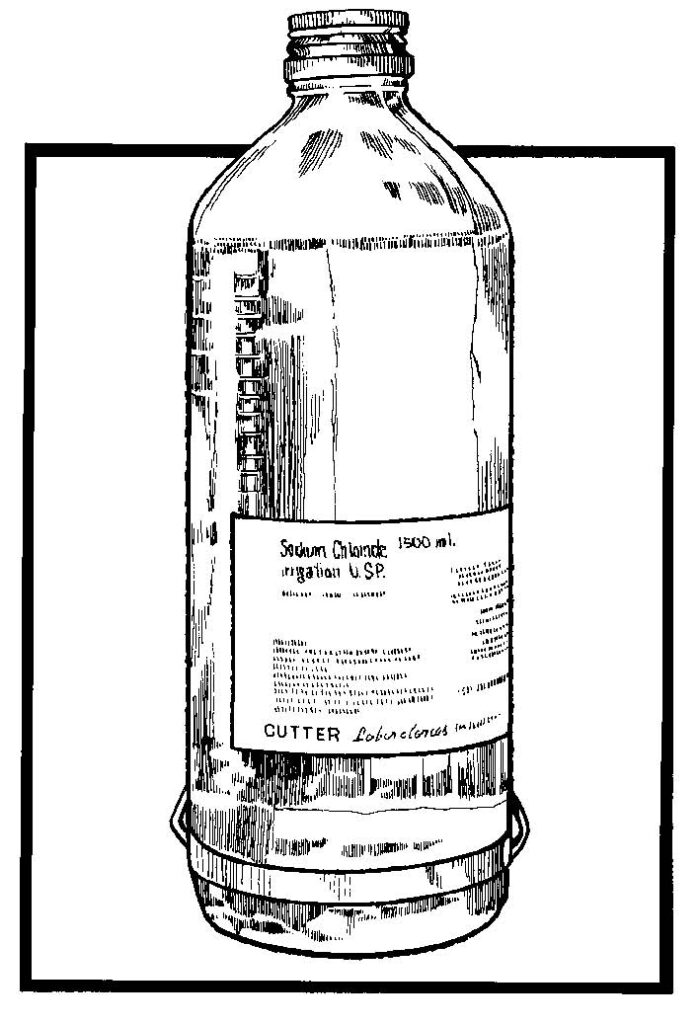
The infusion and irrigator stand (see figure 1-21) is a mobile, adjustable-height stand from which containers of whole blood, intravenous solutions, or irrigating solutions are suspended. At least one stand per OR is needed for the administration of fluids. (See the stand in figure 1-14.) A second intravenously infusion (IV) stand should be available, as it may be needed to serve as an anchor point for the drape, thus separating the anesthetist from the sterile field. Figure 1-22 illustrates commercially prepared irrigating solutions and hospital prepared irrigating solutions.
1-19. SUCTION APPARATUS
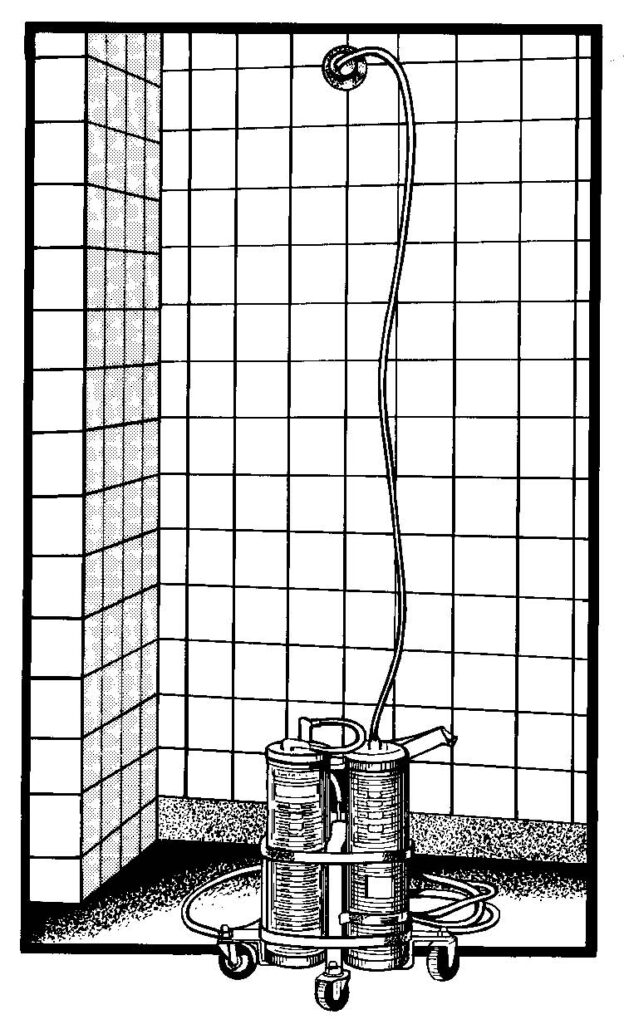
A suction apparatus (see figure. 1-23) is used to siphon blood and other fluids from the body cavities or areas in which the surgeon is operating. Another unit of this type with its attachments is used by the anesthetist. If in-wall suction is available, a suction container with tubing on a low-wheeled base is necessary. Equipment should be tested immediately before low-wheeled base is necessary. Equipment should be tested immediately before each operation. Containers for use with suction apparatus are calibrated so that the drainage can be measured accurately. Additional containers should be available in the room where the suction apparatus is being used.
1-20. SPONGE COUNT BOARD
A small board (see figures. 1-24 and 1-25), sometimes attached to the wall, is used to record the sponge count. The sponge count is recorded on it before surgery begins and whenever called for during the operation.
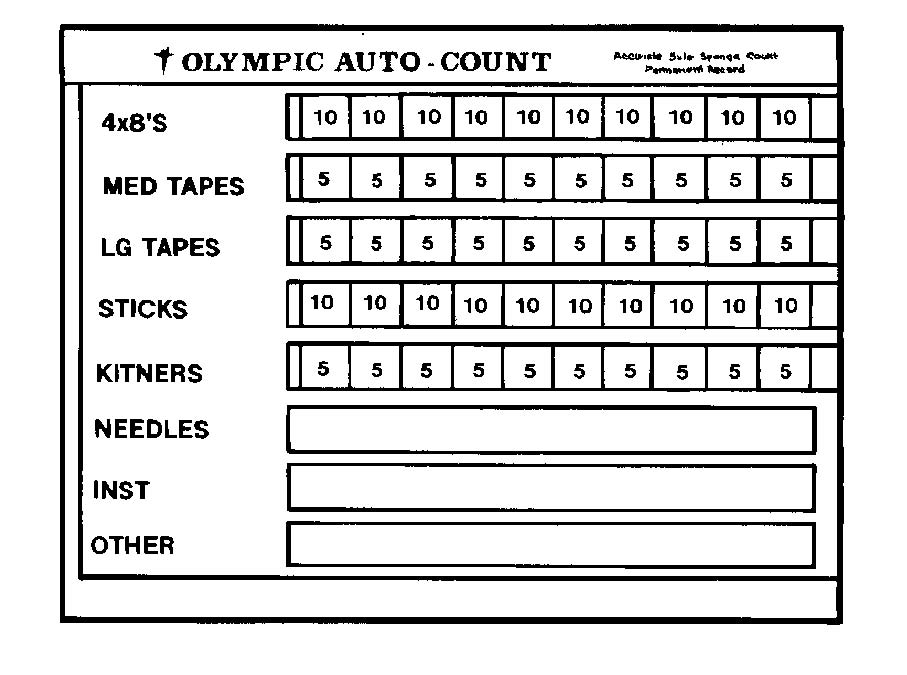
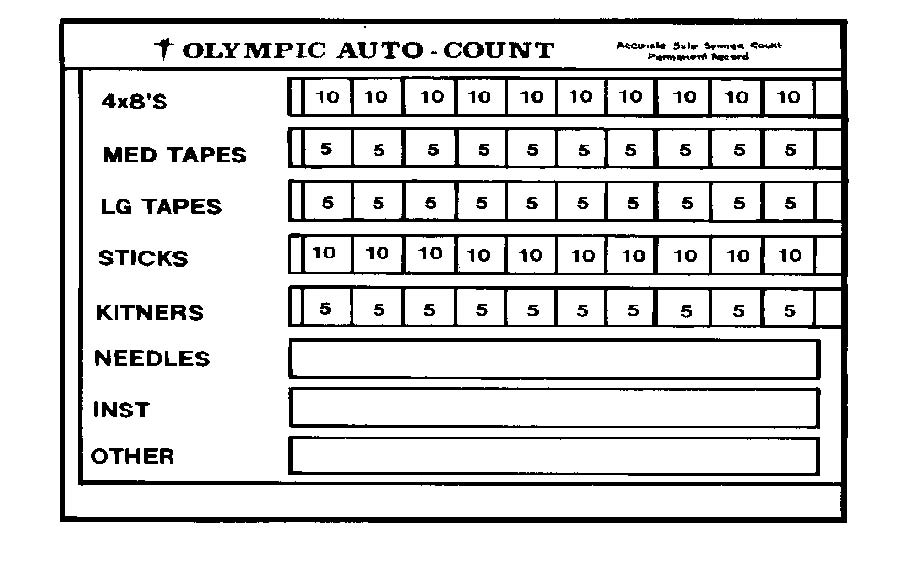
Numbered blocks are uncovered.
1-21. ADDITIONAL EQUIPMENT
a. Endoscopy.
(1) General. Endoscopy is a visual examination of the interior of the body cavity, hollow organ, or structure with an endoscope, an instrument designed for direct visual inspection. The endoscope usually is inserted into a natural body orifice, that is, the mouth, anus, or urethra. It may be inserted through a small skin incision and/or trocar puncture, as through the abdominal or vaginal wall. An endoscopic procedure is designated by the anatomic structure to be visualized.
(2) Light source. Illumination within the body cavity is essential for visual acuity. The light source may be through a fiber-optic bundle or from an incandescent light bulb.
(a) Fiber-optic lighting. This is an improved lighting system that illuminates body cavities, including those that cannot be seen with other light sources. Light is conducted through a bundle of thousands of coated glass fibers encased in a plastic sheath. Electric current must be transmitted to the light source connected to the fiber-optic bundle. With fiber-optic lighting, the electric current is entirely external to the patient.
(b) Bulbs screw into the fitting either at the end of a removable light carrier or at the end of the built-in lens system. Electric current is conducted through a single-filament wire to illuminate the tiny incandescent light bulb. A battery box with one or more sets of dry-cell batteries may be used as the power source for light bulbs. Fiber-optic lighting has replaced bulbs in most endoscopes.
(3) Accessories. Accessories such as suction tubes, snares, biopsy forceps, grasping forceps, electrosurgical tips, sponge carriers, and so forth, are used in conjunction with endoscopes. These can be passed through channels in the endoscope to remove fluid or tissue, coagulated bleeding vessels, inject fluid or gas to distend cavities, and so forth. Lensed scopes may be equipped with a still or motion picture camera so organs or lesions can be photographed during the procedure. Some rigid scopes have an obturator, a blunt-tipped rod placed through the lumen of the scope, to permit smooth insertion of the instrument as into the anus. The accessories that will be needed will be determined by the type of endoscope and the purpose of the procedure.
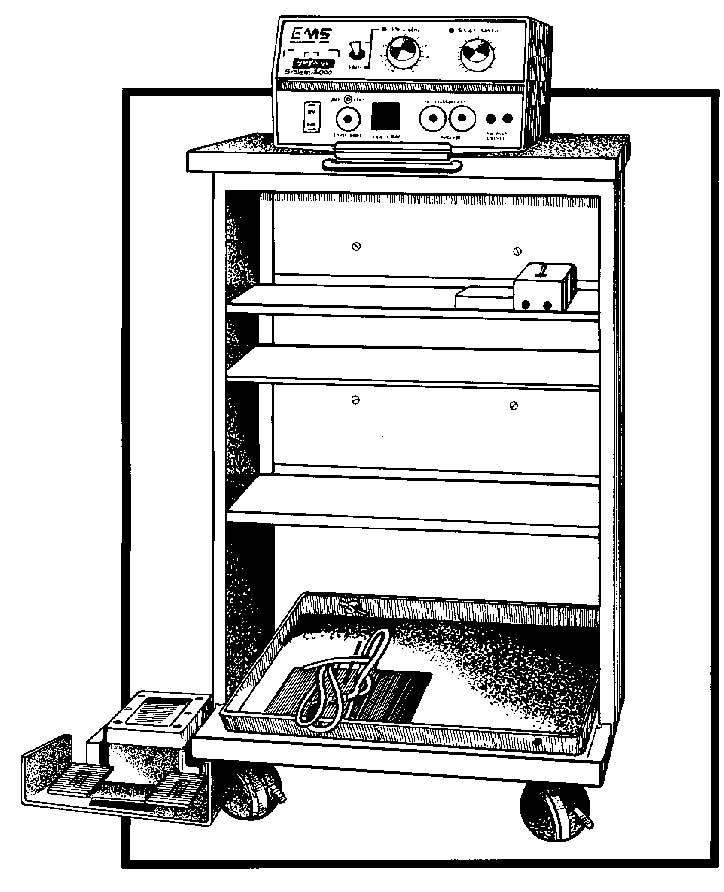
b. Electrosurgical Apparatus. The electrosurgical apparatus (unit) is an electrical machine that has a very high frequency of alternating current. Figure 1-26 shows an electrosurgical apparatus. The surgeon may use the electrosurgical apparatus to do the following procedures: cut body tissue, stop bleeding from small blood vessels (coagulation), destroy abnormal growths such as a wart (fulguration), and sear or dry tissue (desiccation).
(1) Advantages of the use of electro surgery over mechanical (hand) surgery are numerous. A discussion of these follows.
(a) The electrosurgery active electrode (operative tip) can perform two processes simultaneously; it can seal as it cuts. The alternating current makes an incision in an exceedingly fine line. By adjustment of the controls, this unit can also cauterize, or literally cook, the tissue, thus closing (sealing) blood vessels instead of tying each one individually with a suture. These two processes, cutting and sealing, may be done simultaneously or individually. These processes are particularly applicable for use in the presence of cancerous tissue. Removal of malignant growths by mechanical (hand) surgery is dangerous because cells may break off, travel to other parts of the body via the circulatory system, and spread the cancer. However, in electrosurgery, blood vessels are closed as they are cut, preventing the spread of cancer in this way.
(b) Another advantage relates to blood loss. Electrosurgery decreases blood loss. Cauterization is very effective in obtaining hemostasis (arresting the flow of blood). By setting the unit for cauterization, the surgeon need only touch the instrument to the hemostat (clamp which controls bleeding) he has placed on a bleeder and the bleeding is stopped. In mechanical (hand) surgery, each layer of tissue cut requires many hemostats and many ties. Considerable blood is lost while time is taken to tie each bleeder.
(2) The electrosurgerical apparatus has an active electrode and an inactive electrode.
(a) Current passes into the patient’s body through an active electrode, the operative tip. A tip is small in area, concentrating the current; hence, it generates considerable heat where the surgeon applies it. The active electrode and its connecting cord are the only parts of the unit sterilized for the operation. This operative tip used by the surgeon is heated only while it is being used; either by a switch on the active electrode handle or by a foot switch, placed near the operating table.
(b) The electrical circuit is completed with the inactive electrode, a large plate made of CRM. This plate is large so that the energy is spread over a large surface area, such as the buttocks, dispersing the current and producing only negligible heat. The inactive electrode is often placed under the patient’s buttocks because of the fleshy, smooth tissue available there which can provide a good contact. The area used for inactive electrode must be free from scars and excessive hair. Scar tissue is made up of uneven connective tissue, which does not provide good contact. Hair is not conductive and must be removed for a good contact.
In addition, bony portions of the body should not be in contact with the inactive electrode because they provide an uneven current distribution, which may lead to burns. Before the inactive electrode is positioned, it should be covered with contact paste (electrocardiograph electrode paste). This paste facilitates passage of electricity. K-Y lubricating jelly should NOT be used because it is nonelectrolytic and will insulate the electrical contact. This will cause current to pass through the thin portions of the K-Y jelly, thus concentrating the current and causing burns to the patient. Disposable plates that conform to the body are also used.
(3) The OR specialist should read the instructions, usually on a plate on the machine or the instruction booklet appropriate to the machine.
(a) The circulator sets up the unsterile parts of the machine since he is the unsterile member of the team. He must set the controls according to the surgeon’s orders. The circulator also places the foot pedal conveniently for the surgeon’s use.
(b) The scrub sets up the sterile parts and checks the tip to ensure that all parts are present; he inserts the tip into the handle. The scrub hands the end of the cord with the plug to the circulator, who plugs it into the machine.
(c) The unit is tested for proper functioning before the operative procedure begins.
c. Cardiac Arrest Tray.
(1) A sterile cardiac arrest tray is kept in a place easily accessible to the ORs so that it is quickly available should a patient’s heart stop beating during the induction of anesthesia or the course of surgery.
(NOTE: The incidence of cardiac arrest is about 1 in 800 general anesthesia.)
The tray contains the instruments necessary for opening the patient’s chest and retracting his ribs, thus enabling the surgeon to use his hand to pump the patient’s heart. Cardiac arrest is a dire surgical emergency because when the heart stops there is no circulation of blood and therefore no oxygen is available to the tissues. The tissues of the brain are very quickly damaged by anoxia: thus, the time limit for institution of corrective treatment is considered to be from three to five minutes.
(2) In view of the above considerations, Army hospitals require that a preparedness program be in effect. Cardiac arrest trays are therefore located in all areas where anesthesia (either local or general) is administered. All personnel working in such areas must know where the trays are located.