1-4. DEFINITION
The use of the term “operating room” requires clarification. The entire area in which surgical operations are performed and materials are prepared and stored for surgery is properly called the operating room suite or the surgical suite. However, hospital personnel often describe the entire suite simply as the “operating room” (OR). Examples of such usage are: “OR specialist,” “OR nurse,” and “OR supervisor”–all of whom have duties throughout the surgical suite.
Of course, “operating room” and “OR” are also used to indicate an individual OR in which surgery is performed. Throughout this subcourse, these terms “operating room suite” and “surgical suite” are used when referring to the entire area in which operations are performed and supplies are prepared and/or stored. Terms such as “OR specialist,” “OR supervisor,” and “OR personnel” are in general use and are understood by all hospital personnel as referring to persons assigned to the OR suite. The terms “operating room” and “individual operating room” are used to designate a room within the surgical suite where surgery is performed on a patient.
1-5. LOCATION
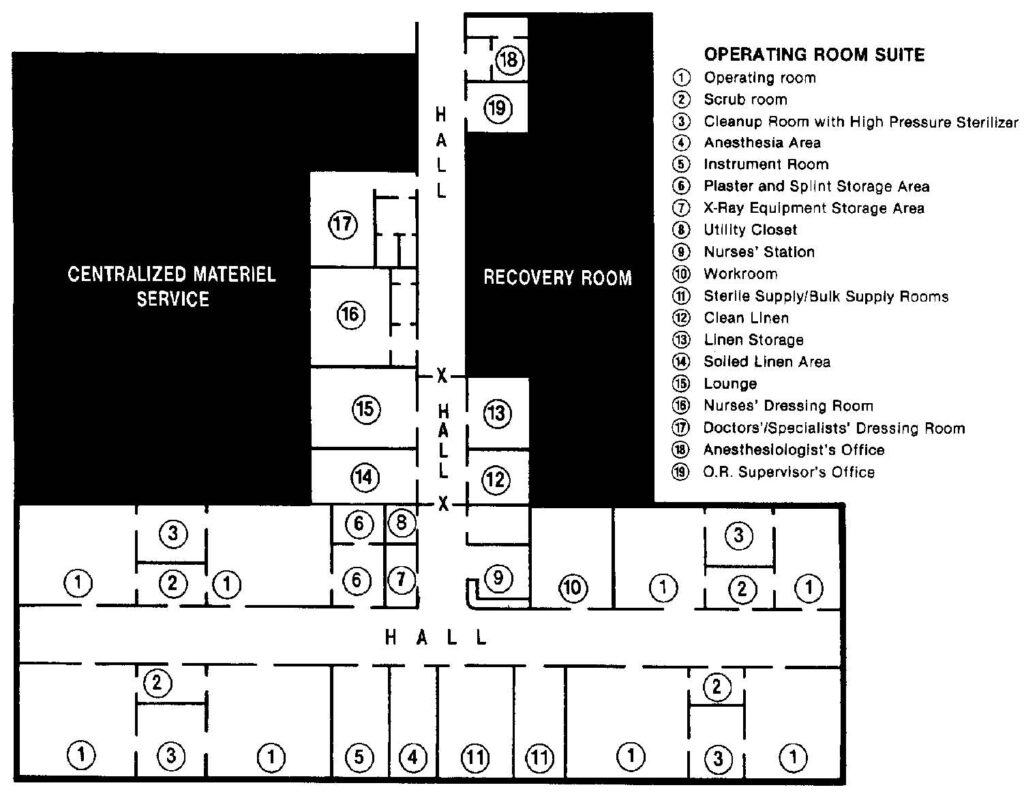
The surgical suite should be centrally located so that it is easily and quickly reached from all areas of the hospital, thus enabling personnel to transfer patients with the least possible delay. The suite should be situated near such support activities as X-ray, laboratory, centralized materiel service (CMS), pharmacy, and the recovery room (see figure 1-3). In addition, the suite should be located in a cul-de-sac (passage with only one outlet), or at least away from those areas of the hospital through which most of the traffic flows and should be sufficiently isolated to prevent annoyance, anxiety, and disturbance to other patients. Elevators should be easily reached for transportation of patients or supplies.
1-6. PHYSICAL LAYOUT
a. Arrangement. Basic principles for efficient workflow are adhered to when planning the arrangement of rooms within a surgical suite. For example, traffic must move smoothly and without interruption into, through, and out of the suite. Those rooms where support activities are performed are grouped conveniently and systematically about the ORs, which are arranged in pairs with scrub rooms and sterilizing facilities between them. (See figure 1-3). Proper arrangement of the rooms reduces the flow of excess traffic, saves much unnecessary walking, and therefore conserves time and effort.
b. Size of the Suite. Numerous factors are considered when estimating the size of the surgical suite required for a hospital.
(1) The first of these is the operative load or the number of surgical cases to be done per day. Some hospitals have more patients requiring medical care than surgical care. In such a hospital, only a small operative section would be necessary. Several operative procedures can be done per day in each OR, one case following another, but all should be completed by the end of the usual day shift or shortly thereafter.
(a) The average number of ORs needed is indicated by the number of operative cases to be done daily divided by the number of cases that can be done daily in one OR.
(b) Operative load can also be broadly interpreted to include the amount of work to be done per day, outside of actual cases. There is a great deal of preparatory work necessary for each surgical procedure as well as the routine tasks to maintain the suite. If most supplies are prepared and sterilized in CMS, the OR suite needs to maintain only a small preparation and sterilization area; otherwise, it may need a large one.
(2) The second factor, the types of surgery to be done, is even more specific. Some procedures such as cardiac surgery are very long and detailed, requiring many hours of operative time; others, such as tonsillectomy, can be accomplished in just 20 to 30 minutes. In the first instance, a single OR would be engaged for the whole operative day with just one case; in the second example, eight or ten such procedures could be done in the same length of time.
(3) The number and frequency of emergency cases are also considerations related to the necessary size of the suite. The larger the troop area near a hospital, the greater the number of accident and emergency cases that may have to be done. These must be done immediately, meaning that other scheduled cases may have to wait until after normal duty hours, unless provision has been made for an additional room.
c. Size of Individual Operating Room. In addition to plans for the number of ORs required, the size of each room must also be considered. Certain types of surgery require the use of much bulky equipment. This is especially true of open-heart surgery, during which large machines are required to pump and oxygenate the blood outside of the body and to monitor the functioning of the heart. Factors such as this must be planned for and sufficient floor space provided so that breaks in aseptic technique due to overcrowding will be avoided. On the other hand, rooms should be no larger than necessary, thus reducing the amount of unnecessary times spent walking. The Army criteria for square footage per room are sufficiently flexible to provide for the needs of its hospitals. (See figure 1-3, “Type” floor plan for an Army hospital-operating suite.)
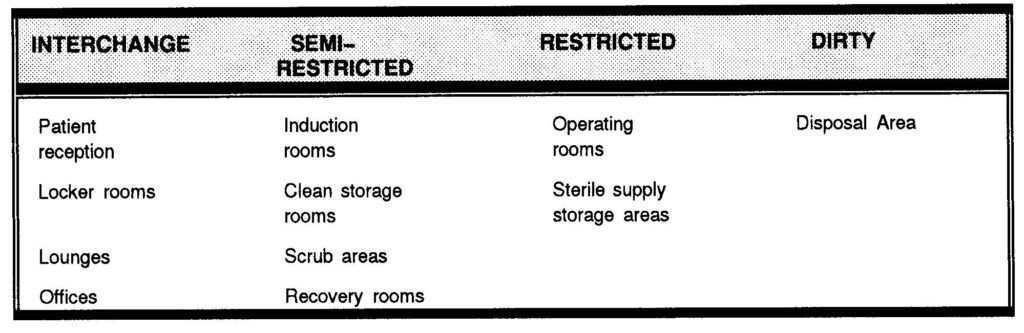
d. Four Areas. The designations listed in the Four Zone Concept (1) thru (4) are not necessarily used for all hospitals, but whenever feasible the surgical suite is segregated into four areas for traffic control. The purpose of such control is to assure maximum protection against infections. In analyzing the traffic and commerce system of the OR system, specific traffic patterns must be determined. These are dependent on the entrances and exits for both personnel and materials. Renovation planning of existing facilities should consider renovation of central supply and storage areas to bring these as close to the point of utilization as possible. Where entirely new wings, buildings, or entire hospital complexes are being considered, there is opportunity to design traffic, materials-handling, and storage systems around the requirements of the surgical suite. Traffic control design is aided by designation of the four-zone concept (as shown below): the interchange area, semirestricted area, restricted area, and dirty area.
(1) Interchange area. The interchange area is provided to enable persons from outside the surgical suite to meet with personnel within the suite when necessary. Examples of such rooms are the offices–one for the OR supervisor and one for the chief of anesthesiology (see figure 1-3 (18) and (19))–whenever the offices for these personnel are situated within the surgical suite. In some hospitals, these offices are located convenient to but outside the surgical suite in order to keep traffic within the suite to a minimum. If there is a postanesthesia (recovery) room, it is also classified as an interchange area although entry is carefully controlled.
The main outer corridors are in the interchange area. This area also consists of the rooms designed for personnel to change from street clothes or military uniforms into OR attire (“scrub clothing”) (see figure 1-3 (15), (16), and (17)). If space and arrangement permit, there are two doors to each dressing room–one for the entry of persons in street clothes and the other for their exit in scrub clothes. The individual lockers are generally equipped with nametags, locks, and keys. Caps, masks, and scrub clothing are stored in the dressing rooms. Dressing rooms may be equipped with showers. A mask need not be worn in this area.
(2) Semirestricted area. Comprising the semirestricted area are corridors within the work area, the anesthesia workroom and storage, the utility closet, the instrument storage room, the workroom, the linen storage room, the clean linen room, and the soiled linen room (see figure 1-3 (4), (5), (7), (8), (10), (11), (12), (13), and (14)). The semirestricted area then represents the supply center for the surgical suite. Although, non-sterile procedures are performed in this area, personnel without OR attire are not admitted. A mask need not be worn in this area.
(3) Restricted area. The restricted area consists of all rooms in which sterile procedures are done and sterile goods are opened or exposed. This includes the individual ORs and the adjacent scrub rooms (see figure 1-3) where soap, nail files, brushes, timers, and written directions are available for the scrub procedure. Also included are the preanesthesia rooms (induction rooms) if the suite has this facility. On the floor plan shown in figure 1-3, a part of the “anesthesia area,” (4), may be designated for the induction of anesthesia. If the suite is arranged to include a substerilizing room between each two ORs (see figure 1-3 (3)), then these rooms are considered to be restricted because supplies are autoclaved here without being covered and are moved, uncovered, into the OR. Each person working in the restricted area is required to wear scrub clothes, cap, and mask.
(4) Dirty area. The dirty area is the disposal area, where all utilized materials and linen are gathered, packaged, and sent to appropriate areas.
e. Arrangement of Areas. There is no one rule that must be followed in the physical arrangement of the four areas previously discussed. However, the nonrestricted and interchange areas should be located near the entry door. Workroom areas are situated near the center of the suite, and storage and supply rooms nearby are positioned to avoid waste in time and energy of personnel. Areas for storage of both sterile and unsterile supplies must be clearly marked to avoid mistaking one for the other. If there is no linen chute in the suite, a room for soiled linen is necessary (see figures 1-3 (14)). This room is classified as semirestricted. If the suite has observation galleries, these are provided with outside entries to eliminate unnecessary traffic of persons in street clothing.
1-7. CONSTRUCTION
a. Discussion. Construction of the individual ORs is important because each room should provide an ideal area for the performance of surgery. In addition, proper construction makes provision for the maximum efficiency of personnel and for the safety of both patients and OR personnel. Proper construction and size are also related directly to ease of cleaning and the maintenance of aseptic technique.
b. Floors. Floors should be smooth, wear-resistant, and nonporous. Suitable materials include ceramic tile, terrazzo, or vinyl plastic approved for installation in the OR by the National Fire Protection Association. Edges and corners at the juncture of floor and walls are rounded to prevent the accumulation of dust and facilitate cleaning. The ceramic tile or other material used for construction of floors is impregnated with a conductive material and is rounded. The purpose of this type of flooring is to provide a path, which will conduct electricity away from all persons and equipment making contact with the floor, thus preventing the accumulation of dangerous electrostatic charges. Conductive flooring for special application rooms is not required where inflammable anesthetic gases are prohibited and where a high degree of monitoring is required.
c. Walls. Walls no longer have to be tiled. The plaster between the tiles is porous and can harbor bacteria. New paneling materials and flexible wall coverings, along with new adhesives, permit completely sealed wall, ceiling, and floor joints so that these surfaces may be washed with all types of bactericidal chemical solutions. However, the walls may be covered completely with nonglare tile. If tiled, the tile should reach at least six feet up from the floor for easy wet-cleaning and scrubbing. The upper portions of the walls are painted with a washable pastel paint the color of the tile.
d. Ceilings. Ceilings are often smooth, washable, and soundproofed. They are often painted the same or similar color as the walls. White is no longer used since colors lessen the glaring reflection of light in the eyes.
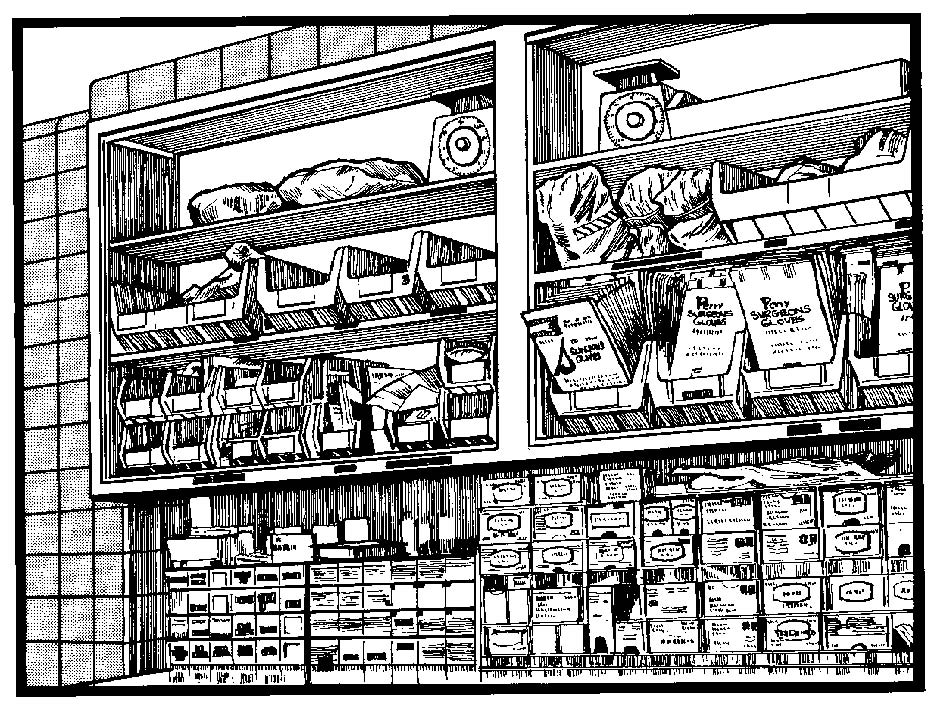
e. Cabinets. Cabinet can be provided for the storage of sutures, medications, infusion sets, and other supplies. If recessed into the walls and provided with sliding doors, these cabinets conserve working space and interfere less with the maintenance of aseptic technique. Cabinets should be in a well-lighted area of the room and should be easily accessible to the circulator who will be required to furnish supplies from them during the operative procedure (see figure 1-4).
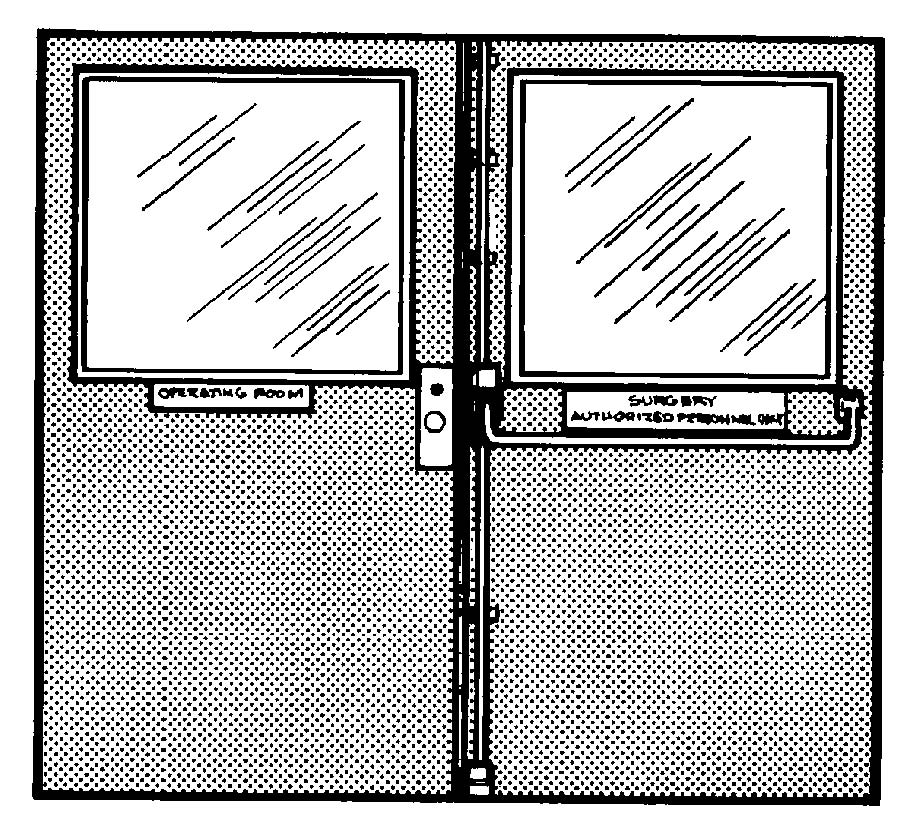
f. Doors. Doors may be of several types. All doorframes should be a minimum of five feet in width. One type of door is the “double acting” (swinging) type with rubberized door guards on each side. These doors should be equipped with a window for easy visualization from both sides (see figure 1-5). A second type is a door, which swings outward. Swinging doors produce air turbulence, which increases bacteria count. However, minimum use of swinging doors is advised
g. Signal Light. Each room should be equipped with an emergency signal light or call button that can be operated conveniently by the anesthetist or circulator.
NOTE: In this subcourse, references to the “scrub” and “circulator” pertain to certain duties performed by the OR specialist. (Refer to lesson 2, paragraph 2-18.)
h. Special Surgical Needs. The Surgical Specialties require consideration of special needs. For example, flush-mounted snap-lock water connections for the heart-lung machine, X-ray facilities, space for neurocryosurgery, and special outlets for air-powered equipment may be required. Some Specialties use fiber optics, a laser apparatus, special built-in television, or cine cameras. Each service is consulted for any anticipated special needs that will require preparation, operation, or maintenance by the nursing service.
1-8. LIGHTING
a. Ordinary lighting for the OR is adequately provided by fixtures recessed into the ceilings. To provide additional light over the operative area, there is a special overhead light fixture (see figure 1-6) suspended from the ceiling. This fixture is designed to provide shadow-free lighting on the operative area, to give off a minimum amount of heat, and to be easily cleaned and adjusted. The specialist should practice adjusting this light so that he can make changes quickly and accurately during surgery. The ceiling lights and the operating lights are on different circuits to avoid confusion and delay if a fuse burns out.

b. Portable lights are necessary for satisfactory illumination in some operative procedures such as vaginal or rectal surgery. Storage battery lights should be provided for emergency lighting during a power failure. These must be inspected, tested, and recharged at frequent intervals, as prescribed by local policy.
1-9. ELECTRICAL FIXTURES
a. Discussion. In rooms where explosion hazards exist, circuits supplying electrical current for lighting and for wall outlets are all grounded to a common ground to prevent arcs and sparks and to reduce the possibility of electrical shocks to personnel.
b. Outlets. Explosion-proof outlets for mobile equipment are located in the walls about one foot from the floor and also near the operating table. The alternating current (AC) and direct current (DC) outlets are clearly marked by color and shape to prevent plugging a piece of electrical apparatus into the wrong current. These wall outlets have interlocking switches so that a plug cannot be withdrawn or inserted while a plug is securely inserted into the outlet. The current is broken into an explosion-proof enclosure before the plug is removed. Outlets and switches, which are not explosion-proof are mounted five feet above the floor, in areas where flammable anesthetic agents are administered to patients, because the area is considered to be hazardous up to that level. In some surgical suites, even those outlets that are nonexplosion-proof are mounted five feet from the floor.
c. Extension Cords. Extension cords that are not explosion-proof are never to be used to connect mobile equipment to wall outlets because such cords are hazardous. The foot control pieces for mobile electrical equipment are insulated as a precaution against explosion.
d. Other Fixtures. Other items of electrical equipment usually included are vapor-proof X-ray view boxes built directly into the wall and an explosion-proof electric wall clock with a sweep second hand.
(1) Operating room suites of the future will be designed to facilitate the use of computers in the monitoring of patients, in obtaining diagnostic data and calculations, and in the ordering of supplies. Hospital designers may plan for computer terminals to be directly accessible to specially trained individuals who can interpret the data in the OR.
(2) All cabinets, view boxes, and receptacles should be recessed. Wall-mounted shelves and mounted cabinets, and freestanding storage cabinets are being used less and less because of difficulty in cleaning and maintaining supplies.
(3) The current trend is toward the cart system where mobile units are constantly supplied and cleaned.
(4) No windows should be installed.
1-10. TEMPERATURE, HUMIDITY, AND AIR CIRCULATION
Ventilation should be furnished by an air-conditioning system whenever possible. Hence, it should be relatively easy to provide a regulated temperature of 72ºF to 78ºF. Humidity should be maintained between 55 and 60 percent to lessen the explosion hazard when flammable anesthetic agents are administered. Air conditioning also assists in the elimination of foreign particles by providing freshly filtered air free of dust.