2-27. EPISTAXIS
Nosebleed, called epistaxis, is caused by the rupture of the tiny blood vessels in the nose. Most often, the vessels ruptured are those in the mucous membranes of the nose.
a. Epistaxis may be caused by injury, such as a blow to the nose, “picking” the nose, or forceful blowing of the nose. Nosebleed may also occur as the result of disease or may occur as a symptom of conditions such as sinusitis, bleeding disorders, or hypertension.
b. Epistaxis can often be managed conservatively by compressing the nostril of the affected side against the nasal septum for 5-10 minutes. A cold compress over the nose is also effective in the reduction of both bleeding and swelling. Position the patient with the head forward to allow blood to drain from the nose and not down the throat. Swallowing the blood may lead to nausea and vomiting. Instruct the patient to breathe through the mouth. If the source of the bleeding cannot be seen, the physician may spray the interior of the nose with an epinephrine solution, which will constrict the blood vessels, and pack the interior of the nose with gauze, which will act as a pressure dressing.
2-28. ALLERGIC RHINITIS
Rhinitis is the inflammation of the mucous membrane of the nose. Allergic rhinitis is a general term used to describe any allergic reaction of the nasal mucosa.
a. Non-seasonal (perennial) allergic rhinitis is an allergic rhinitis that may occur intermittently or continuously all year round. It is caused by exposure to an allergen such as house dust, animal dander, or food. It is characterized by sudden attacks of sneezing, swelling of the nasal mucosa with watery discharge, and itching of the eyes with lacrimation.
b. Seasonal allergic rhinitis (hay fever) is a seasonal variety of allergic rhinitis caused by a specific allergen such as a particular pollen. It is characterized by acute conjunctivitis with itching and lacrimation, swelling of the nasal mucosa with watery discharge, sudden attacks of sneezing, and quite often with asthmatic symptoms.
2-29. SINUSITIS
Inflammation of a sinus may be acute or chronic. It usually occurs with other upper respiratory infections since mucous membranes of the nasal cavities are continuous with the sinuses. Sinusitis may also occur from obstructions that block drainage from the sinuses. An untreated acute sinusitis may become chronic or may lead to a more serious condition such as brain abscess, meningitis, or septicemia.
a. Sinusitis is characterized by pain and nasal congestion. The location of the pain is diagnostically important. Frontal pain or headache indicates frontal sinus involvement. Pain in and around the eyes is associated with the ethmoid sinuses. Maxillary sinusitis is characterized by pain lateral to the nose, sometimes accompanied by aching in the upper teeth. In sphenoid sinusitis, an occipital headache may occur.
b. Treatment involves rest and measures to facilitate sinus drainage. Increased humidity, increased fluid intake, and steam inhalation will help to liquify and loosen secretions. Nasal and/or oral use of vasoconstricting drugs is indicated. Antihistimines and antibiotics may also be used depending upon the causative agents involved.
2-30. PHARYNGITIS
Inflammation of the pharynx is caused by several viruses and bacteria. It is characterized by pain in the throat, dysphagia, red and inflamed mucosa, and enlargement of the tonsils and cervical lymph nodes.
a. Throat culture is used to determine the causative organism. If the condition is caused by bacteria such as streptococcus or staphylococcus, the symptoms may be more severe and complications such as sinusitis, mastoiditis, and otitis media may occur.
b. Treatment involves warm saline gargles and irrigations. An ice collar may be used to reduce pain and swelling. Analgesic and antitussive medications are given to alleviate pain and coughing. Antibiotics will be prescribed for a bacterial causative organism.
c. Because of throat discomfort and difficulty swallowing, the patient should be given a soft or liquid diet while symptoms are severe. Fluids should be encouraged.
2-31. TONSILITIS
Tonsilitis is inflammation of the palatine tonsils, a pair of lymphatic tissue structures, and one located on each side of the oropharynx. Enlargement of the adenoids, a large mass of lymphoid tissue at the posterior wall of the nasopharynx, often accompanies acute tonsilitis.
a. Symptoms include a painful and inflamed throat, difficulty swallowing, and enlarged tonsils with exudate that appears as white or yellow spots.
b. Treatment includes warm throat irrigations and analgesics. A throat culture at the tonsillar site is done to determine the type of bacteria present, and antibiotic therapy is initiated.
c. Tonsillectomy and adenoidectomy are indicated when treatment is unsuccessful and antibiotics cannot control frequent recurrent infections or when hypertrophy or peritonsillar abscess threaten to occlude the airway.
2-32. LARYNGITIS
Inflammation of the larynx, or voice box, is most commonly caused by voice abuse, excessive use of tobacco, or as a result of infection.
a. It is characterized by a sore and dry throat, cough, and hoarseness or loss of voice.
b. Treatment involves voice rest and restriction from smoking. Steam inhalation therapy is often indicated. Antibiotic therapy should be initiated if the laryngitis is a result of bacterial infection.
2-33. ACUTE CORYZA
The “common cold” is the term used to refer to afebrile, infectious, acute coryza, which is caused by many different viruses. Colds are highly contagious. Symptoms do not appear until 24-48 hours after exposure to the virus, yet during this time the exposed individual is already contagious.
a. Symptoms may include nasal congestion and discharge, sneezing, sore throat, fever, chills, and malaise. Nasal congestion causes pressure that results in headache. As a cold progresses, a cough may develop. Symptoms last about 1-2 weeks if the infection remains uncomplicated.
b. Treatment is symptomatic, involving the use of analgesics, decongestants, and expectorants. Warm salt-water gargles may relieve sore throat pain. Adequate rest, plenty of fluids, and vitamin C are routinely included in the treatment of a cold.
2-34. CARE FOLLOWING SURGERY OF THE NOSE
a. Surgery of or through the nose may be required to correct the results of trauma to the nose and related structures; to correct deformities that interfere with breathing, such as a deviated septum, hypertrophy of the turbinates, or polyps; and to relieve the effects of sinusitis. Surgery of the nose may also be done for cosmetic reasons.
b. Epistaxis is usually the most serious complication of surgery of the nose. If bleeding occurs postoperatively, attempt to control the bleeding with compression of the nostrils and utilization of cold compresses. If nasal packing is in place, bloody sputum or bloody vomit may be considered signs of nasal bleeding. The nursing personnel must be alert for excessive or continuous bleeding, restlessness, breathing irregularities, cyanosis, and tachycardia. If these signs and symptoms are noted, the professional nurse must be notified immediately. If the physician must be called, make ready a head mirror, light, nasal speculum, packing forceps, and packing material.
c. Quite often, the patient’s nose will be packed at the termination of the surgery. This may cause an intense fear of suffocation. The patient must be reassured that mouth breathing will supply sufficient air. Continued mouth breathing will cause dryness of the lips and mouth. Ointment such as petrolatum should be applied to the patient’s lips and fluids given as tolerated to moisten the mouth. The patient may have the urge to blow his nose to relieve the sense of fullness caused by the packing. Instruct the patient not to blow his nose, as this may cause bleeding and would be ineffective in relieving the sense of fullness.
2-35. TONSILLECTOMY AND ADENOIDECTOMY
a. Removal of the tonsils and adenoids is indicated in cases of recurrent infections or in cases of swelling that threatens to obstruct the airway.
b. Postoperative nursing management involves maintenance of a patent airway and observation for bleeding and aspiration.
(1) If the operation was done under a local anesthetic, place the patient in a sitting position to maintain airway patency.
(2) If the operation was done under general anesthesia, place the patient in a lateral recumbent position with the head extended. This will allow drainage through the nose and mouth.
(3) Observe vital signs closely and be alert for changes that may indicate bleeding, such as gurgling respirations or excessive swallowing.
(4) Keep the patient as quiet as possible.
(5) Place an ice collar around the neck to constrict blood vessels and reduce pain.
c. An unconscious or bleeding patient should never be left alone. Suction equipment should be available for use. If suctioning is necessary, it should be done carefully and gently to avoid disturbing the operative sites.
d. Encourage the patient to take the diet prescribed by the physician. For the first few days the diet will probably be liquid or semisolid. All foods and fluids should be bland, avoiding citrus, acidic foods, and spices. Diet should be advanced as patient tolerance dictates.
e. Utilize prescribed analgesics, since the throat will be sore for several days postoperatively.
2-36. LARYNGECTOMY
a. Surgery of the larynx is done most often to remove a tumor or growth that may be malignant.
(1) A malignant growth may occur on the vocal cords (intrinsic) or on another part of the larynx (extrinsic). The type of surgery done depends upon the location and involvement of the growth.
(2) Newly developed surgical procedures are being used in the management of laryngeal growths. Some procedures involve resection of the larynx or formation of an air passage from the trachea to the pharynx. The objective of these procedures is to preserve the voice.
b. Partial laryngectomy is the removal of that portion of the vocal cord that is involved with abnormal growth. A tracheostomy tube may be left in the neck wound for a few days postoperatively. The neck wound will eventually heal, and the normal respiratory system and voice are preserved.
c. Total laryngectomy is the removal of the larynx, vocal cords, thyroid cartilage, and the epiglottis. The trachea is sutured to the anterior surface of the neck as a permanent tracheostomy. The patient breathes exclusively through the neck opening (stoma) and is referred to as a total neck breather, since the airway between the mouth, nose, and throat has been completely closed.
(1) Total laryngectomy with laryngoplasty involves the formation of a tube that leads from the upper trachea to the lower pharynx. This “speaking” tube allows for speech that sounds almost normal. A patient having this type of laryngectomy is referred to as a partial neck breather, since the tube allows the passage of air from the nose and mouth into the trachea.
(2) When the patient has a total laryngectomy, the surgeon will most likely place a laryngectomy tube in the newly formed stoma. This tube may be removed when the stoma has healed, usually within 4-6 weeks. The laryngectomy tube is shorter, but larger in diameter, than a tracheostomy tube. Care of the laryngectomy tube is the same as that for the tracheostomy tube.
(3) Since the patient will not be able to speak initially, some means of communication must be developed for the patient. Commonly used techniques are simple note writing, flash cards, magnetic letter boards, and magic slates. Always have a call bell within the patient’s reach. When the stoma has healed, the speech pathologists will work with the patient to help him learn new speaking methods.
d. Special considerations for the laryngectomee include the following:
(1) For the laryngectomee, air passes directly into the trachea without being moistened and warmed by the upper respiratory mucosa. This causes the trachea and bronchi to secrete excessive amounts of mucous, and the patient may experience frequent bouts of coughing. In time, the mucosa of the trachea and bronchi will adapt to this altered physiology. In the meantime, however, the patient will be more comfortable with added humidification in the inspired air. This may be provided by steam or cool mist humidifiers.
(2) Precautions must be taken in the shower to prevent water from entering the stoma. A small plastic bib worn around the neck works well. Swimming is not recommended, as the laryngectomee may drown without ever putting his face in the water.
(3) Care must be taken to prevent hair spray, powder, loose hairs, and any other foreign objects from entering the stoma.
(4) A laryngectomee should carry or wear identification that will alert a first-aid giver to his special resuscitation needs. A laryngectomy stoma may be hidden by a scarf and not noticed by the first-aid giver. A neck breather, whether partial or total, requires artificial ventilation through the stoma. This may be done by mouth-to-stoma artificial respiration or by bag-mask to stoma. If the patient wears a tube in his stoma, do not remove it. Give artificial ventilation through it. The mouth and nose must be sealed closed to prevent the escape of air from the nose and mouth, in the event that the patient is a partial neck breather.
2-37. TRACHEOSTOMY
a. A tracheotomy is the incision of the trachea through the skin and muscles of the neck. When an indwelling tube is inserted into the surgically created opening in the trachea, the term “tracheostomy” is used. A tracheostomy may be permanent or temporary. There are many diseases and conditions that make a tracheostomy necessary. For example, a tracheostomy may be done:
(1) To bypass an upper airway obstruction.
(2) To replace an endotracheal tube with a tracheostomy tube.
(3) To allow for extended mechanical ventilation.
(4) To facilitate removal of tracheobronchial secretions.
(5) To prevent aspiration in the comatose or paralyzed patient.
b. A tracheostomy tube (sometimes referred to as a tracheal cannula set) consists of three parts: the outer cannula, the inner cannula, and the obturator. Refer to Figure 2-3.
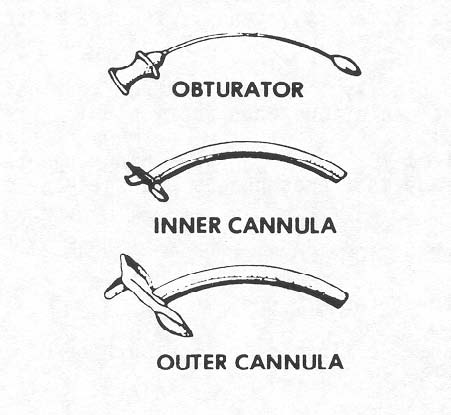
(1) The obturator is used by the surgeon as a guide when inserting the outer cannula into the tracheal incision.
(2) After insertion of the outer cannula, the obturator is removed. The inner cannula is inserted into the outer cannula and locked in place.
(3) Tracheostomy tubes may be metal or plastic. Plastic tubes that have an inflatable cuff surrounding the outer cannula are the most commonly used. The cuff helps to hold the tube in place, prevents aspiration of material into the lungs, and prevents leaking of air around the sides of the tube.
(4) The tracheostomy tube is kept in place by means of cotton twill tape inserted through the slotted flanges of the outer cannula and tied around the patient’s neck. A sterile dressing is placed around the tube to protect the stoma.
2-38. TRACHEOSTOMY NURSING CARE
a. Preparatory Nursing Measures. In addition to routine preparation of the patient unit for postoperative care, the following measures should be planned in advance.
(1) The patient will require constant attendance for at least the first 48 hours. The nursing personnel must remember two important things: the patient’s life depends upon a clear airway, and the patient will have a temporary loss of voice. Therefore, the patient must be observed closely for airway patency and immediate action taken when any adverse signs or symptoms are present. The patient will feel anxious about his inability to communicate with his voice. Always have the call bell available to the patient. Devise a temporary means of communication such as writing notes or using flash cards so that the patient may communicate his needs to the nursing personnel.
(2) For the first few days postoperatively, the patient should be kept in a room where the temperature and humidity can be maintained at optimum levels. Increased temperature and humidity will help to reduce the tracheal irritation that results when inspired air has bypassed the natural warming and moisturizing of the nasopharyngeal airway.
(3) The patient’s room should be supplied with a variety of equipment necessary to the care of the patient. Such things include suction equipment, a spare tracheostomy tube set, and sterile dressing material.
b. Postoperative Nursing Measures. In addition to routine postoperative nursing care, the following nursing actions should be noted.
(1) Always apply basic principles of aseptic technique when caring for the incision and the airway. When suctioning, use separate set-ups for pharyngeal and tracheostomy suctioning.
(2) Constantly observe the patient for signs of respiratory obstruction such as restlessness, cyanosis, increased pulse, or gurgling noises during respiration.
(3) Watch closely for bleeding from the incision, and look for blood in the aspirated secretions when suctioning.
(4) Be alert for choking or coughing when the patient swallows. This may indicate damage to the esophagus with leakage of swallowed material into the trachea.
2-39. PERFORMING TRACHEOSTOMY SUCTIONING
a. Assemble the necessary equipment.
(1) Portable continuous suction machine or in-wall suction.
(2) Sterile suction kit containing sterile suction catheters (14-18ºFr.), a sterile solution container, and sterile gloves.
(3) Sterile saline in a pour bottle.
(4) Sterile gauze sponges.
(5) Sterile normal saline in 5cc packets for tracheal instillation, if ordered.
(6) Oxygen source with flow meter and a manual resuscitator (ambu bag).
(7) Waste receptacle.
b. Explain the suctioning procedure to the patient if he is conscious.
(1) Hyper oxygenation will be performed. An ambu bag with 100 percent oxygen will be connected to the tracheostomy tube and the patient will be given several breaths prior to suctioning. This is done to prevent shortness of breath or hypoxia.
(2) Approximately 5cc of normal saline will be instilled into the tracheostomy tube to help liquify secretions. Inform the patient that this may stimulate a cough reflex.
c. Place the patient in semi-Fowler’s position if permitted.
d. Wash your hands and set up the sterile suction kit.
(1) Open the suction kit, using the wrapper to create a sterile field. Place the sterile sponges on the field.
(2) Pour 50-100cc of sterile saline into the solution container, using a septic technique.
e. Turn on the suction unit and set to low pressure to avoid trauma to the patient.
f. Using aseptic technique, don the sterile gloves.
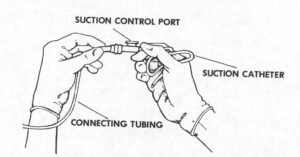
g. Attach the sterile suction catheter to the connecting tubing by holding the catheter in your dominant hand (sterile hand) and the connecting tube in your non-dominant hand (non-sterile hand). Refer to Figure 2-4.
h. Moisten the catheter tip in the sterile saline.
i. Instruct your assistant to hyper oxygenate the patient.
(1) Disconnect ventilator tubing if patient is receiving mechanical ventilation.
(2) Give the patient several breaths of 100 percent oxygen with the ambu bag and quickly remove the bag.
j. With the suction diverted, gently insert the sterile suction catheter into the tracheostomy tube until slight resistance is felt, then pull back slightly.
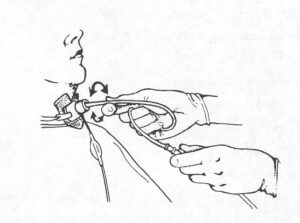
k. Apply suction.
(1) Place the thumb of your non-dominant (non-sterile) hand over the suction control port of the catheter.
(2) Rotate the catheter between the thumb and index finger of your sterile hand while withdrawing the catheter. Apply intermittent suction while withdrawing.
(3) Suction only for 5-10 seconds. Refer to Figure 2-5.
l. Instruct the assistant to hyper oxygenate the patient while you rinse the catheter by suctioning a small amount of the sterile saline.
m. If secretions are thick, instill 5 cc of sterile normal saline into the tracheostomy tube and suction again.
n. Repeat the suction procedure until the airway is clear.
(1) Hyper oxygenate the patient between suctioning.
(2) Rinse the catheter between suctioning.
o. Reconnect the patient to the ventilator if one is in use.
p. Perform oropharyngeal suctioning, if required.
q. Discard used equipment and restock the patient’s bedside with new equipment.
r. Record the procedure in the Nursing Notes.
2-40. PERFORMING TRACHEOSTOMY CARE
Changing the tracheostomy dressing, cleansing the skin around the stoma, and cleaning the inner cannula are collectively referred to as tracheostomy care.
a. Assemble necessary equipment and supplies.
(1) Trach cleaning kit (obtain from CMS).
(2) Clean scissors.
(3) Hydrogen peroxide.
(4) Sterile saline–pour bottle.
(5) Sterile gloves–2 pairs.
(6) Exam gloves–2.
(7) Waste receptacle.
b. Explain the procedure to the patient and establish a method of communication.
c. If suctioning is required, perform that procedure prior to beginning tracheostomy care. It is routine to perform tracheostomy care after suctioning.
d. Position the patient in semi-Fowler’s position if permissible.
e. Wash your hands and set up the equipment using aseptic technique.
(1) Open the cleaning kit, using wrapper as a sterile field.
(2) Open dressings and other supplies and place on sterile field.
(3) Pour hydrogen peroxide in one basin and sterile saline in the other (disposable basins/containers are included in the kit).
f. Put on exam gloves and remove soiled tracheostomy dressing. Tracheostomy secretions should be considered contaminated and handled accordingly.
g. Remove and discard exam gloves and put on sterile gloves.
h. Clean inner cannula, if present.
(1) Unlock the inner cannula and remove.
(2) Place the inner cannula in the hydrogen peroxide, allowing it to soak for a few minutes.
(3) Clean the inner cannula with the test tube brush.
(4) Rinse the inner cannula in the sterile saline.
(5) Remove the inner cannula from the saline and allow it to drain on a sterile 4×4 gauze sponge.
i. Cleanse the tracheostomy incision and surrounding area with antiseptic swabs.
(1) If crusting occurs, remove with sterile swabs soaked in hydrogen peroxide.
(2) Do not allow cleansing solutions to enter the tracheostomy opening.
j. Reinsert the inner cannula and lock in place.
k. Apply sterile tracheostomy dressing. Use precut, non-raveling sterile 4×4. Place it with the slit toward the chin, allowing the uncut portion to absorb secretions.
l. Reapply ties.
(1) Cut and remove soiled, outer tube ties if necessary. The patient or an assistant should hold the outer tube in place to prevent dislodgement of the tube.
NOTE: If an assistant is not available and the ties must be changed, secure new ties in place before cutting and removing soiled ties.
(2) Cut a slit about one inch from the end of each tape.
(3) Insert the slit end of the tape through the flange of the outer cannula, and draw the other end of the tape through the slit (Figure 2-6).
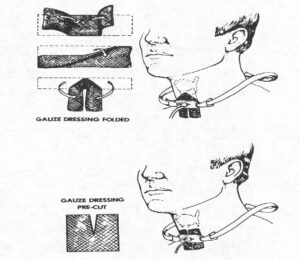
(4) Tie the tapes securely with a knot, never a bow. Position the knot at the side of the patient’s neck rather than the back. Trim off excess tape.
m. Remove and discard gloves or return all equipment to the appropriate location.
n. Record procedure in Nursing Notes.
