2-23. THORACENTESIS
a. General. Thoracentesis is the procedure in which a puncture is made into the chest wall to withdraw fluid or air from the pleural cavity for diagnostic or therapeutic purposes. A thoracotomy needle is inserted through the intercostal area into the pleural cavity. Suction is then applied by syringe to aspirate the accumulated fluid or air. The procedure is usually done at the patient’s bedside.
b. Assembling the Necessary Equipment. Assemble the following:
(1) Sterile thoracentesis tray (obtain from CMS).
(2) Calibrated drainage bottle.
(3) Sterile gloves.
(4) 4×4 gauze compresses.
(5) Prescribed local anesthetic.
(6) Alcohol prep sponges.
(7) Adhesive tape.
(8) Mobile table or stand.
(9) Waste receptacle.
c. Preparation for the Procedure.
(1) Check clinical record for signed SF 522 (Authorization for Administration of Anesthesia and for Performance of Operations and Other Procedures).
(2) Obtain chest X-rays, if requested.
(3) Explain the procedure to the patient, stressing the importance of remaining immobile during the procedure.
(4) Take and record TPR and blood pressure (BP).
(5) Screen the patient. Remove pajama jacket to expose chest. The site of the puncture will depend upon the location of the fluid or air that is to be aspirated.
(6) Position the patient as directed by the physician. The position may be either one of the following or a similar position, as directed by the physician.
(a) Seat the patient on the side of the bed, facing away from the physician, with feet supported on a chair and the head and arms resting on an overbed table padded with pillows. The arms are elevated slightly to widen the intercostal spaces.
(b) Place the patient in a semi recumbent position, facing away from the physician, resting on the non-affected side, with the head of the bed elevated about 45 degrees. A pillow is placed under the chest to widen the intercostal spaces. The arm of the affected side is placed above the head to elevate the ribs, thereby making the insertion of the needle easier.
d. Assisting with Thoracentesis.
(1) Place the thoracentesis tray on instrument table. Open sterile wrapper cover to provide a sterile field.
(2) Place other supplies on adjacent bedside stand or over bed table. Open glove wrapper.
(3) Assist with handling of local anesthetic vial. Hold vial with label uppermost so that the physician can personally check the label before withdrawing any of the solution. Cleanse stopper with alcohol sponge. Invert vial and hold firmly while the doctor, with gloved hands, withdraws the required solution.
(4) Support and help patient to avoid moving and coughing while the thoracentesis needle is introduced.
(5) Assist as directed with collection of specimens as the physician manipulates the syringe, the stopcock, and drainage tubing. Use care not to contaminate the end of the tubing, the cap, or the open end of the specimen tubes. Cap the tubes and place them upright in a clean glass provided for this purpose. Label each tube as directed by the physician.
(6) If drainage of a large amount of accumulated fluid is necessary, assist the doctor by placing the free end of the tubing in the drainage bottle.
(7) Watch the patient’s color; check pulse and respiration. Immediately report any sudden change, as this may indicate damage to the visceral pleura from a nick or puncture by the needle.
(8) After the needle is withdrawn, apply a sterile dressing over the puncture site.
(9) Position patient comfortably (usually Fowler’s position).
e. Follow-up Procedures.
(1) Remove equipment from bedside to utility room.
(2) Complete entries on appropriate laboratory request forms as directed.
(3) Send properly labeled specimens with completed request forms to laboratory immediately.
(4) Measure and record amount of fluid withdrawn and discard this fluid unless directed otherwise.
(5) Discard disposables, place all linen in hamper, and return appropriate items to CMS.
(6) Continue to observe patient for respiratory difficulty: persistent cough, dyspnea, or the presence of blood in the sputum. Take and record vital signs q4h (every 4 hours), or as ordered.
(7) Obtain post-procedural chest X-rays, if ordered.
(8) Enter the following information on Nursing Notes: date and time, procedure, by whom performed, amount and type of fluid withdrawn, patient’s reactions, and specimens sent to laboratory.
2-24. CHEST TUBE INSERTION
a. General. Chest tube insertion (tube thoracotomy) is the insertion of one or more flexible tubes into the pleural space to remove air, blood, or fluid. This procedure is done by the physician.
b. Assembling the Necessary Equipment. Assemble the following:
(1) Thoracotomy tray (obtain from CMS).
(2) Sterile gloves.
(3) Padded hemostats.
(4) Suture material.
(5) Local anesthetic.
(6) Chest tube and connector.
(7) Chest drainage system: connecting tubing and collection bottles, or commercial system.
(8) Suction apparatus (if ordered).
(9) Mobile table or stand.
c. Preparation for the Procedure.
(1) Explain the procedure to the patient.
(2) Obtain and record vital signs.
(3) Assemble the drainage system.
(4) Set up and test the suction apparatus if one is ordered.
(5) Screen the patient and remove pajama coat to expose the chest. The insertion site will depend upon the presence of air or fluid.
(6) Position the patient as directed by the physician.
d. Assisting with Chest Tube Insertion.
(1) Set up the thoracotomy tray on the instrument table, using sterile technique.
(2) Using sterile technique, place other supplies on the sterile field.
(3) Assist the physician with the skin prep and administration of local anesthetic as for thoracentesis.
(4) Assist the physician with tube insertion, as directed. There are varying methods of introducing a tube into the pleural space. The method used depends upon the size of the tube to be inserted, the equipment available, and the physician’s preference.
(5) The physician connects the patient’s chest tube and the drainage tubing, checks the entire system to verify all connections, and tapes the connections to ensure an airtight system. He will then unclamp the chest tube. The clamps are never removed until the drainage system is airtight and ready to function.
(6) The chest tube is normally sutured in place and covered with a sterile dressing.
(7) Arrange for a follow-up chest X-ray, if ordered.
e. Follow-up Procedures.
(1) Remove equipment from bedside and care for properly.
(2) Observe patient for respiratory difficulty.
(3) Continue to observe the drainage system for proper function.
(4) Tape the padded hemostats and a package of sterile vaseline gauze to the head of the patient’s bed. This equipment must be available for emergency use should the chest tube become dislodged or the drainage system opened.
(5) Record the procedure in the Nursing Notes. Note the patient’s tolerance to the procedure.
2-25. WATER-SEAL CHEST DRAINAGE
a. General. Underwater-seal chest drainage is a closed (airtight) system for drainage of air and fluid from the chest cavity.
(1) The underwater-seal system is established by connecting a catheter (chest tube) that has been placed in the patient’s pleural cavity to drainage tubing that leads to a sealed drainage bottle.
(2) Air and fluid drain into the bottle, but water acts as a seal to keep the air from being drawn back into the pleural space.
(3) By keeping the drainage bottle at floor level, fluid will be prevented from being siphoned back.
(4) As air and fluid are drained, pressure on the lungs is relieved and re-expansion of the lung is facilitated.
b. Selection of the System. The physician will specify the drainage setup he prefers to use. It is a nursing responsibility to be familiar with the various systems and their operation.
(1) When the physician specifies his preference, the nursing personnel will obtain, assemble, and check the system, maintaining asepsis within the system.
(2) Chest drainage can be organized into three types of systems. Each can be used with or without suction. Refer to Figure 2-2 as you read the descriptions that follow.
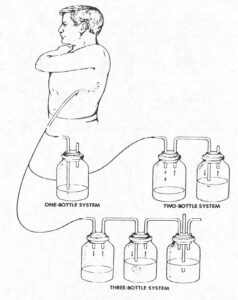
c. The Single-Bottle Water-Seal System.
(1) Connecting or drainage tubing joins the patient’s chest tube with a drainage tube (glass rod) that enters the drainage bottle.
(2) The end of the glass rod is submerged in water, extending about 2.5 cm (1 inch) below the water level.
(3) The water seal permits drainage of air and fluid from the pleural space but does not allow air to reenter the chest.
(4) Drainage depends upon gravity, the mechanics of respiration, and, if ordered, the addition of controlled suction.
(5) The second tube in the drainage bottle is a vent for the escape of any air drained from the lung. If suction is ordered, it is attached here.
(6) Bubbling at the end of the drainage tube may or may not be visible. Bubbling may mean persistent air leaking from the lung or a leak in the system.
(7) The water level in the bottle fluctuates as the patient breathes. It rises when the patient inhales and lowers when the patient exhales.
(8) Since fluid drains into this bottle, be certain to mark the water level prior to opening the system to the patient. This will allow correct measurement of patient drainage.
d. The Two-Bottle Water-Seal System.
(1) The two-bottle system consists of the same water-seal bottle plus a fluid collection bottle.
(2) Pleural fluid accumulates in the collection bottle, and not in the water-seal bottle (as in the single-bottle system).
(3) Drainage depends upon gravity or the amount of suction added to the system.
(4) When suction is added, it is connected at the vent tube in the water-seal bottle.
e. The Three-Bottle Water-Seal System.
(1) This system consists of the water-seal bottle, the fluid collection bottle, and a third bottle which controls the amount of suction applied.
(2) The third bottle, called the manometer bottle, has three tubes. One short tube above the water level comes from the water-seal bottle. A second short tube leads to the suction. The third tube extends below the water level and opens to the atmosphere outside the bottle. It is this tube that regulates the suction, depending upon the depth the tube is submerged. It is normally submerged 20 cm (7.6 inches).
(3) The suction pressure causes outside air to be sucked into the system through the tube, creating a constant pressure. Bubbling in the manometer bottle indicates the system is functioning properly.
f. Commercial Systems.
There are several disposable commercial drainage systems available. They are plastic devices, divided into chambers for fluid collection, water-seal, and suction control. Follow the manufacturer’s instructions for commercial drainage systems used at your facility.
2-26. CARING FOR THE PATIENT WITH WATER-SEAL CHEST DRAINAGE
a. When using suction with water-seal drainage, the system should be open to the atmosphere when the suction is turned off for any reason. This will allow intrapleural air to escape from the system. To do this, simply detach the tubing from the suction port to create an air vent.
b. Observe the water-seal chest drainage system for patency to ensure that it is functioning properly.
(1) Fluid in glass rod (or water seal chamber of commercial devices) should rise and fall with respirations.
(2) Fluctuation should continue until the lung has re-expanded.
c. Observe amount, color, and consistency of chest drainage at ordered time intervals and record results in patient’s clinical record.
(1) Notify charge nurse immediately if chest drainage exceeds 100 cc/hour.
(2) Notify charge nurse immediately if chest drainage color changes to indicate an active bleeding problem.
(3) Mark the level of drainage on a piece of adhesive tape affixed to the drainage system every shift, or as ordered; include date, time, and your initials.
(4) Do not empty the drainage system unless directed to do so by the physician.
d. Observe drainage tubing for any kinking.
(1) Do not allow drainage tubing to loop below drainage system entry level.
(2) Fasten the tubing to the draw sheet with rubber bands and safety pins so the flow by gravity will occur.
e. Milk the chest tube, as ordered by the physician, in the direction of chest drainage to promote chest tube patency.
(1) Lubricate the drainage tubing with lubricant (water-soluble) for approximately 12 inches.
(2) Pinch the tubing above the lubrication with one hand; with the other hand compress the tubing, allowing the fingers to slide over the lubrication toward the drainage bottle and release both hands.
pressure, crepitus, and/or hemorrhage.
f. Observe the patient carefully for any signs of respiratory difficulty, cyanosis, chest pressure, crepitus, and/or hemorrhage.
(1) Monitor vital signs every 4 hours, or as ordered, and record.
(2) Auscultate patient’s lung sounds every 4 hours and record findings.
g. Check to see that the drainage bottle is secured to the floor or is in a special holder.
(1) Prevent bottle from being kicked or tipped over.
(2) Caution visitors against handling equipment.
h. Observe the dressing at the chest tube insertion site for air leakage or excessive drainage and record findings.
(1) Dressing changes are performed only according to physician’s orders.
(2) Observe skin condition during dressing changes and record.
i. Encourage the patient to cough and deep breath at least every 2 hours or as ordered.
(1) Patient should be assisted to a sitting position if possible to promote effective deep breathing and coughing.
(2) A pillow or blanket should be used to splint the affected area.
j. Encourage the patient to change position every 2 hours to promote drainage and prevent complications; make sure tubing remains free from kinks and is in proper position.
k. Encourage the patient to perform range of motion exercises for the affected upper extremity to maintain joint mobility.
l. Transport or ambulate a patient with a chest tube carefully, keeping the water-seal unit below chest level and upright at all times.
(1) Assist or instruct personnel from other departments in transporting or ambulating the patient.
(2) Nursing staff should accompany the patient.
(3) Disconnect the closed chest drainage system from suction for transportation or ambulation; make sure air vent rod is open.
(4) Attach hemostats (Kelly Clamps) to the patient’s hospital gown during transportation or ambulation for emergency use.
m. As indicated, provide emergency care to the patient if the water- seal unit becomes broken or emptied.
(1) Clamp the chest tube unless there has been a large air leak; chest tube with a large air leak should be left open, since clamping may cause a rapid pneumothorax.
(2) Reestablish a closed drainage system.
(3) Remove clamps, if applied.
(4) Notify the professional nurse/physician, as indicated.
(5) Observe the patient for respiratory distress.
n. As indicated, provide emergency care to the patient if the chest tube becomes disconnected from the drainage system.
(1) Clamp the chest tube.
(2) Cleanse the end of the tubing with an antiseptic solution and reconnect or cut off the contaminated tips of the chest tube and tubing and insert a sterile connecting piece.
(3) Securely tape the connection.
(4) Notify the professional nurse/physician, as indicated.
(5) Observe the patient for respiratory distress.
o. As indicated, provide emergency care to the patient if the water- seal unit is tipped over.
(1) Return unit to upright position.
(2) Instruct the patient to deep breathe and cough to force air out of the pleural space.
(3) Notify the professional nurse.
(4) Assess the patient for respiratory distress.
p. As indicated; provide emergency care to the patient whose chest tube has accidentally been pulled out of the chest wall.
(1) Cover the site with sterile 4″x4″ gauze sponges and tape occlusively.
(2) Notify the professional nurse/physician immediately.
(3) Monitor the patient for respiratory distress.
q. Record significant nursing observations in the patient’s clinical record and report the same to the professional nurse.
(1) Amount, color, and consistency of chest drainage.
(2) Presence or absence of air leaks or bubbling in the water-seal unit.
(3) Presence or absence of fluctuation in the glass rod of the water-seal unit.
(4) Time and results of chest tube milking. Specific observations about the patient, such as vital signs, breathe sounds, and skin color.
(5) Results of deep breathing and coughing.
(6) Position changes or activity, including range of motion.
(7) Condition of chest tube insertion site and dressing.
