1-1. INTRODUCTION
The circulatory system has two major fluid transportation systems, the cardiovascular (CV) 00system and the lymphatic system.
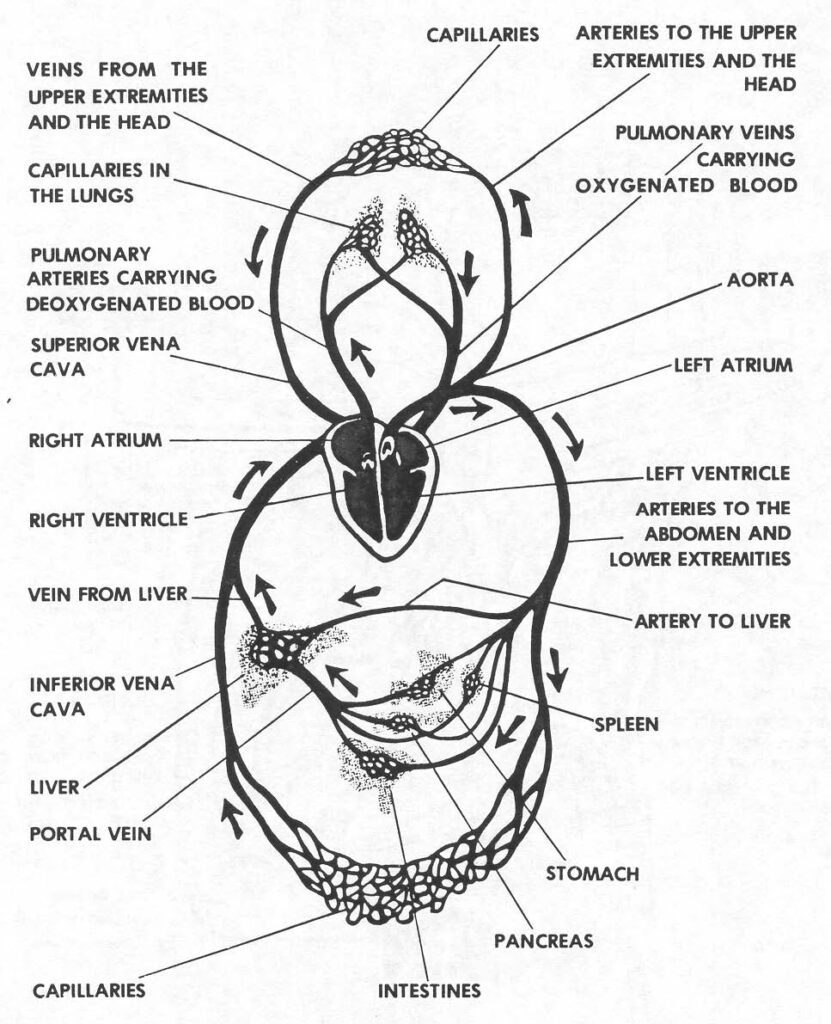
a. Cardiovascular System. This system, which contains the heart and blood vessels, is a closed system, transporting blood to all parts of the body. Blood flowing through the circuit formed by the heart and blood vessels (see Figure 1-1) brings oxygen, food, and other chemical elements to tissue cells and removes carbon dioxide and other waste products resulting from cell activity.
b. Lymphatic System. This system, which provides drainage for tissue fluid, is an auxiliary part of the circulatory system, returning an important amount of tissue fluid to the blood stream through its own system of lymphatic vessels.
1-2. THE HEART
The heart, designed to be a highly efficient pump, is a four-chambered muscular organ, lying within the chest, with about 2/3 of its mass to the left of the midline. It lies in the pericardial space in the thoracic cavity between the two lungs. In size and shape, it resembles a man’s closed fist. Its lower point, the apex, lies just above the left diaphragm. Refer to Figure 1-2 as you continue to read.
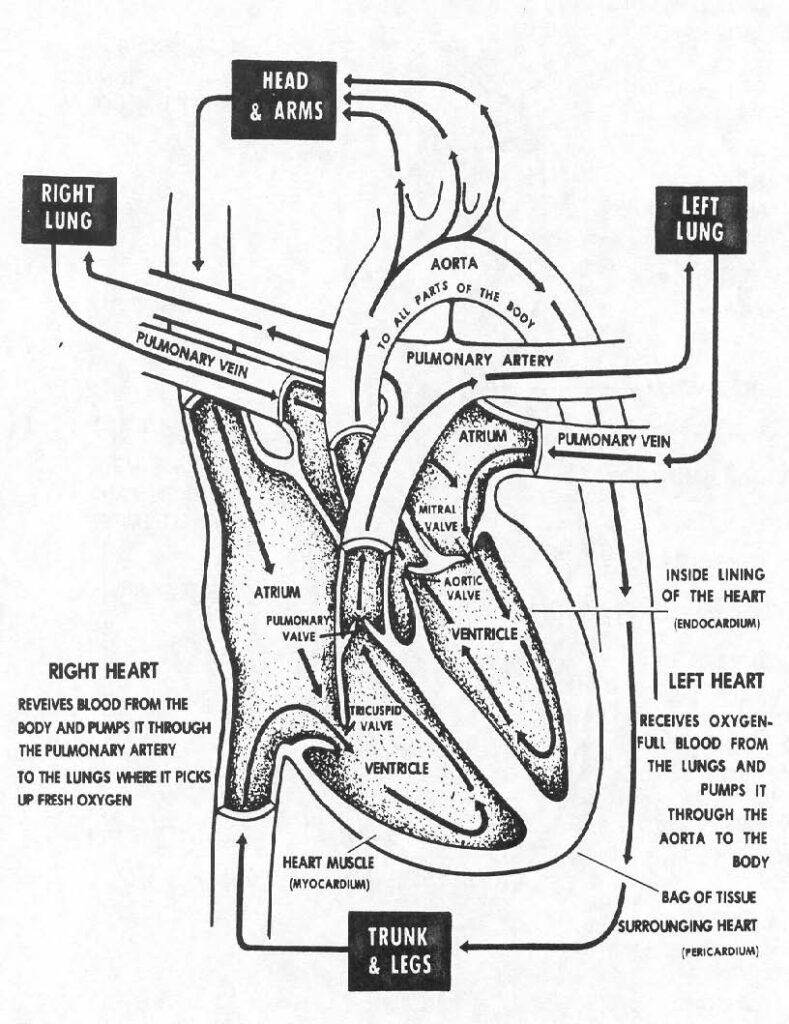
a. Heart Layers. The pericardium is a double walled sac enclosing the heart. The outer fibrous surface gives support, and the inner lining prevents friction as the heart moves within its protecting jacket. The lining surfaces of the pericardial sac produce a small amount of pericardial fluid needed for lubrication to facilitate the normal movements of the heart.
b. Heart Wall. The walls of the heart is composed of three distinct layers an outer epicardium- which corresponds to the visceral pericardium it protects the heart by reducing friction, a middle layer the myocardium consist mostly of cardiac muscle tissue that pumps blood out of the heart chambers, an inner layer endocardium consist of epithelium and connective tissue that contains many elastic and collagenous fibers.
c. Heart Chambers. There are four chambers in the heart. These chambers are essentially the same size. The upper chambers, called the atria, are seemingly smaller than the lower chambers, the ventricles. The apparent difference in total size is due to the thickness of the myocardial layer. The right atrium communicates with the right ventricle; the left atrium communicates with the left ventricle. The septum (partition), dividing the interior of the heart into right and left sides, prevents direct communication of blood flow from right to left chambers or left to right chambers. This is important, because the right side of the heart receives un-oxygenated blood returning from the systemic (body) circulation. The left side of the heart receives oxygenated blood returning from the pulmonary (lung) circulation. The special structure of the heart keeps the blood flowing in its proper direction to and from the heart chambers.
d. Heart Valves. The four chambers of the heart are lined with endocardium. At each opening from the chambers this lining folds on itself and extends into the opening to form valves. These valves allow the blood to pass from a chamber but prevent its return. The atrioventricular valves, between the upper and lower chambers, are within the heart itself. The semilunar valves are within arteries arising from the right and left ventricles.
(1) Atrioventricular valves. The tricuspid valve is located between the right atrium and right ventricle. It has three flaps or cusps. The bicuspid valve or mitral valve is located between the left atrium and left ventricle. It has two flaps or cusps.
(2) Semilunar valves. The pulmonary semilunar (half-moon shaped) valve is located at the opening into the pulmonary artery that arises from the right ventricle. The aortic semilunar valve is located at the opening into the aorta that arises from the left ventricle.
1-3. FLOW OF BLOOD THROUGH THE HEART
It is helpful to follow the flow of blood through the heart in order to understand the relationship of the heart structures. Remember, the heart is the pump and is also the connection between the systemic circulation and pulmonary circulation. All the blood returning from the systemic circulation must flow through the pulmonary circulation for exchange of carbon dioxide for oxygen. Blood from the upper part of the body enters the heart through the superior vena cava and blood from the lower part of the body enters through the inferior vena cava.
a. Blood from the superior vena cava and inferior vena cava enters the heart at the right atrium. The right atrium contracts, and blood is forced through the open tricuspid valve into the relaxed right ventricle.
b. As the right ventricle contracts, the tricuspid valve is closed, preventing back flow into the atrium. The pulmonary semilunar valve opens as a result of the force and movement of the blood, and the right ventricle pumps the blood into the pulmonary artery.
c. The blood is carried through the lung tissues, exchanging its carbon dioxide for oxygen in the alveoli. This oxygenated blood is collected from the main pulmonary veins and delivered back to the left side of the heart to the left atrium.
d. As the left atrium contracts, the oxygenated blood flows through the open bicuspid (mitral) valve into the left ventricle.
e. As the left ventricle contracts, the bicuspid valve is closed. The aortic semilunar valve opens as a result of the force and movement of the blood, and the left ventricle pumps oxygenated blood through the aortic semilunar valve into the aorta, the main artery of the body. Oxygenated blood now starts its flow to all of the body cells and tissues. The systemic circulation starts from the left ventricle, the pulmonary circulation from the right ventricle.
1-4. BLOOD AND NERVE SUPPLY OF THE HEART
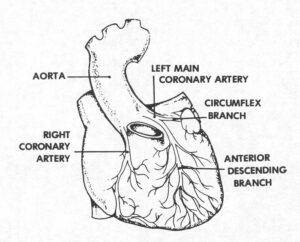
a. Coronary Arteries. The heart gets its blood supply from the right and left coronary arteries (Figure 1-3). These arteries branch off from the aorta just above the Aortic Valve, then subdivide into many smaller branches within the heart muscle. If any part of the heart muscle is deprived of its blood supply through interruption of blood flow through the coronary arteries and their branches, the muscle tissue deprived of blood cannot function and will die. This is called myocardial infarction (MI). Blood from the heart tissue is returned by coronary veins to the right atrium via the coronary sinus.
b. Nerve Supply. The nerve supply to the heart is from two sets of nerves originating in the medulla of the brain. The nerves are part of the involuntary (autonomic) nervous system. One set, the branches from the vagus nerve, keeps the heart beating at a slow, regular rate. The other set, the cardiac accelerator nerves, speeds up the heart. The heart muscle has a special ability; it contracts automatically, but the nerve supply is needed to provide an effective contraction for blood circulation. Within the heart muscle itself, there are special groups of nerve fibers that conduct impulses for contraction. These groups make up the conduction system of the heart. When the conduction system does not operate properly, the heart muscle contractions are uncoordinated and ineffective. The impulses within the heart muscle are tiny electric currents, which can be picked up and recorded by the electrocardiogram, the ECG.
1-5. BLOOD VESSELS
The blood vessels are the closed system of tubes through which the blood flows. The arteries and arterioles are distributors. The capillaries are the vessels through which all exchange of fluid, oxygen, and carbon dioxide takes place between the blood and tissue cells. The capillaries are the smallest of these vessels but are of greatest importance functionally in the circulatory system. The venules and veins are collectors, carrying blood back to the heart.
a. The Arteries and Arterioles. The system of arteries and arterioles is like a tree, with the large trunk, the aorta, giving off branches that repeatedly divide and subdivide. Arterioles are very small arteries, about the diameter of a hair. By way of comparison, the aorta is more than one inch in diameter. An artery wall has a layer of elastic, muscular tissue that allows it to dilate and constrict. When an artery is cut, this wall does not collapse, and bright red blood escapes from the artery in spurts.
b. Capillaries. Microscopic in size, capillaries are so numerous that there is at least one or more near every living cell. A single layer of endothelial cells forms the walls of a capillary. Capillaries are the essential link between arterial and venous circulation. The vital exchange of substances between the capillary blood and the tissue cells takes place through the capillary wall. Blood starts its route back to the heart as it leaves the capillaries.
c. Veins. Veins have thin walls and valves. Formed from the inner vein lining, these valves prevent blood from flowing back toward the capillaries. Venules, the smallest veins, unite into veins of larger and larger size as the blood is collected for return to the heart. The superior vena cava, collecting blood from all regions above the diaphragm and the inferior vena cava, collecting blood from all regions below the diaphragm, return the venous blood to the right atrium of the heart. Superficial veins lie close to the surface of the body and can be seen through the skin.
1-6. PULSE AND BLOOD PRESSURE
a. Pulse. This is a characteristic associated with the heartbeat and the subsequent wave of expansion and recoil set up in the wall of an artery. Pulse is defined as the alternate expansion and recoil of an artery. With each heartbeat, blood is forced into the arteries causing them to dilate (expand). Then the arteries contract (recoil) as the blood moves further along in the circulatory system. The pulse can be felt at certain points in the body where an artery lies close to the surface. The most common location for feeling the pulse is at the wrist, proximal to the thumb on the palm side of the hand (radial artery). Alternate locations are in front of the ear (temporal artery), at the side of the neck (carotid artery), and on the top (dorsum) of the foot (dorsalis pedis).
b. Blood Pressure. The force that blood exerts on the walls of vessels through which it flows is called blood pressure. All parts of the blood vascular system are under pressure, but the term blood pressure usually refers to arterial pressure. Pressure in the arteries is highest when the ventricles contract during systole. Pressure is lowest when the ventricles relax during diastole. The brachial artery, in the upper arm, is the artery usually used for blood pressure measurement.
1-7. LYMPHATIC SYSTEM
The lymphatic system consists of lymph, lymph vessels, and lymph nodes. The spleen belongs, in part, to the lymphatic system. Unlike the cardiovascular system, the lymphatic system has no pump to move the fluid that collects, but muscle contractions and breathing movements aid in the movement of lymph through its channels and its return to the blood stream.
a. Lymph and Tissue Fluid. Lymph, fluid found in the lymph vessels, is clear and watery and is similar to tissue fluid, which is the colorless fluid that fills the spaces between tissues, between the cells of organs, and between cells and connective tissues. Tissue fluid serves as the “middleman” for the exchange between blood and body cells. Formed from plasma, it seeps out of capillary walls. The lymphatic system collects tissue fluid, and as lymph, the collected fluid is started on its way for return to the circulating blood.
b. Lymph Vessels. Starting as small blind ducts within the tissues, the lymphatic vessels enlarge to form lymphatic capillaries. These capillaries unite to form larger lymphatic vessels, which resemble veins in structure and arrangement. Valves in lymph vessels prevent backflow. Superficial lymph vessels collect lymph from the skin and subcutaneous tissue; deep vessels collect lymph from all other parts of the body. The two largest collecting vessels are the thoracic duct and the right lymphatic duct. The thoracic duct receives lymph from all parts of the body except the upper right side. The lymph from the thoracic duct drains into the left subclavian vein, at the root of the neck on the left side. The right lymphatic duct drains into a corresponding vein on the right side.
c. Lymph Nodes. Occurring in groups up to a dozen or more, lymph nodes lie along the course of lymph vessels. Although variable in size, they are usually small oval bodies that are composed of lymphoid tissue. Lymph nodes act as filters for removal of infective organisms from the lymph stream. Important groups of these nodes are located in the axilla, the cervical region, the sub maxillary region, the inguinal (groin) region, and the mesenteric (abdominal) region.
d. Infection and the Lymphatic System. Lymph vessels and lymph nodes often become inflamed as the result of infection. An infection in the hand may cause inflammation of the lymph vessels as high as the axilla (armpit). A sore throat may cause inflammation and swelling of lymph nodes in the neck (submandibular nodes below the jaw and cervical nodes posteriorly).
e. Spleen. The largest collection of lymphoid tissue in the body, the spleen is located high in the abdominal cavity on the left side, below the diaphragm and behind the stomach. It is somewhat long and ovoid (egg- shaped). Although it can be removed (splenectomy) without noticeable harmful effects, the spleen has useful functions, such as serving as a reservoir for blood and red blood cells.
