1-44. FRACTURES
a. A fracture is defined as a break in the continuity of a bone. Fractures occur when a bone is subjected to more stress than it is able to absorb. Fractures may occur from several specific causes and are categorized as follow.
(1) Direct force. In direct force fracture, a bone is subjected to more stress than it can absorb from an impact with a solid object. For example: a direct blow, as from a baseball bat, or a crushing force, such as some automobile accidents.
(2) Twisting. In a twisting (torsion) fracture, an indirect force may cause a break in a bone at a location other than the site of the twisting force. This type of injury is common in skiing accidents.
(3) Muscle contraction. In another indirect force fracture, powerful contraction of a muscle may cause the muscles to tear away from the bone, often fracturing or avulsing part of the bone in the process. This type of injury may occur during a grand mal seizure. This type fracture is seen in soldiers in an injury known as “grenade thrower’s fracture.” The humerus is fractured as a result of the muscular contractions in throwing a hand grenade.
(4) Pathological fracture. Bones that have become weakened from age or disease are easily fractured, often from just a slight movement.
(5) Fatigue or stress fracture. This type of injury may occur when a bone has been subjected to repeated stress. This phenomenon is commonly associated with sports enthusiasts and soldiers. The repeated stress of sustained running or marching may cause stress fractures of the feet or lower extremities.
b. Sometimes it will be quite obvious that a bone is fractured, but this is not always the case. An X-ray will often be necessary to make the diagnosis of fracture. Specific signs and symptoms will vary according to the type and location of the fracture. An open fracture with bone protruding from the wound is very obvious. In the case of a closed fracture, however, a fracture will be more difficult to assess. Some signs and symptoms associated with fractures are:
(1) Pain.
(2) Deformity (visible or palpable).
(3) False motion; abnormal mobility at the fracture site.
(4) Discoloration.
(5) Edema.
(6) Crepitus.
(7) Loss of function.
(8) Shortening of an extremity.
1-45. CLASSIFICATION OF FRACTURES
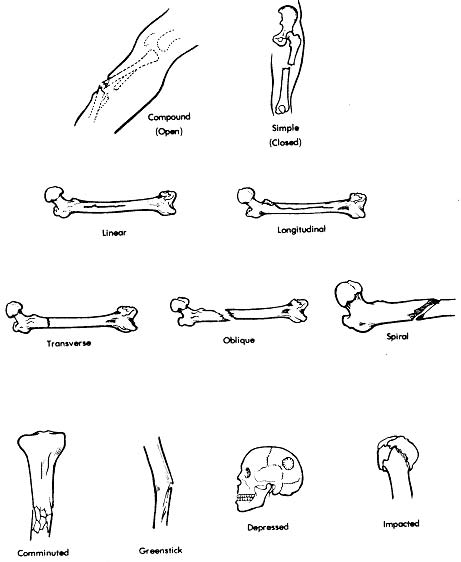
a. A great amount of soft tissue damage often accompanies a fracture. A fracture that is associated with a large amount of nerve, blood vessel, and soft tissue damage is called a complicated fracture. A fracture without other damage would be referred to as an uncomplicated fracture. The nature and extent of the damage depends upon the type and direction of the force causing the fracture. The direction of the force that causes the injury will also determine the direction of the fracture line. The following terms describe the direction of the fracture line in relation to the bone’s longitudinal axis.
(1) Linear. A fracture line that runs parallel to the bone’s axis.
(2) Longitudinal. A fracture line that runs along the length of, but not parallel to, the bone’s axis.
(3) Transverse. A fracture line that runs across, or at a right angle to, the bone’s axis.
(4) Oblique. A fracture line that slants across the bone.
(5) Spiral. A fracture line that runs across the bone at an oblique angle and coils or spirals around the bone.
b. Fractures are primarily classified as open or closed.
(1) Open. An open, or compound fracture is one in which there is an open wound associated with the fracture site.
(2) Closed. In a closed, or simple fracture, there is no break in the skin associated with the fracture.
c. Fractures are further classified according to the condition of the bone, as described below.
(1) Complete. The bone is completely broken or split apart.
(2) Incomplete. The bone is not completely split and part of the bone remains intact.
(3) Displaced. The bone ends are separated at the fracture line and are completely out of alignment.
(4) Impacted or compressed. The bone ends are wedged or jammed into each other.
(5) Depressed. A piece of bone is driven inward, as in a skull fracture.
(6) Comminuted. The bone shatters or fragments into several pieces.
(7) Greenstick. An incomplete fracture in which the bone is partially broken and partially bent. It is similar in appearance to a piece of “green” wood when broken.
d. There are other classification terms associated with fractures, such as identifying a fracture by its location on the shaft of a bone (distal, midshaft, or proximal), or identifying fractures by the name of the physician who first identified them (Colles’, Pott’s, and so forth). Any of the classification terms may be used together to better describe a particular fracture. For example: An open, complicated, complete, comminuted fracture would be one in which the bone is completely broken and fragmented with an associated break in the skin and involvement of nerves, blood vessels, and soft tissue. Refer to figure 1-19 to study the illustrations of these classification terms.
1-46. HEALING OF BONE
a. Bone healing follows an orderly sequence, and it begins the same as wound healing in any other part of the body. When a bone is fractured, hemorrhage between and around the bone ends will occur. Within 24 hours, a blood clot will form. This blood clot is invaded by cells that form granulation tissue. The cells in the newly formed granulation tissue differentiate and form a union of fibrous tissue known as a soft callus. This
soft callus forms a “bridge” between the broken bone ends. Bone-forming cells begin to grow within the soft callus and the soft callus is gradually formed into a hard callus (ossification). There is then a firm bony union between the broken ends of the bone. In treating a fracture, the bones are brought into proper alignment and immobilized until X-rays show that a hard callus has formed.
b. Many factors influence the healing time of fractures and certain conditions may interfere with healing. If the realignment is poor, the bone ends may not meet or there may be soft tissue interposed between the bone ends. Union will not occur under such circumstances. Likewise, if the immobilization is inefficient, union may not occur. The age and physical condition of the patient, as well as dietary deficiencies, will affect the healing time. Additional factors in healing time are the type of fracture, its location, and the adequacy of the blood supply to the affected area. Finally, the presence of infection will severely handicap healing or prevent it altogether.
1-47. PRINCIPLES OF FRACTURE MANAGEMENT
a. In treating a fracture, the objectives of the treatment are as follows:
(1) To regain and maintain the normal alignment of the injured part.
(2) To regain normal function of the injured part.
(3) To achieve the above objectives for the patient in the shortest time possible.
b. The principles of fracture management are reduction, immobilization, and rehabilitation.
(1) Reduction. Reduction is the process of restoring the bone ends (and any fractured fragments) into their normal anatomical positions. This is accomplished by open or closed manipulation of the affected area, referred to as open reduction and closed reduction.
(a) Closed reduction is accomplished by bringing the bone ends into alignment by manipulation and manual traction. X-rays are taken to determine the position of the bones. A cast is normally applied to immobilize the extremity and maintain the reduction.
(b) In open reduction, a surgical opening is made, allowing the bones to be reduced manually under direct visualization. Frequently, internal fixation devices will be used to maintain the bone fragments in reduction.
(2) Immobilization. Immobilization is necessary to maintain fracture reduction until healing occurs. Immobilization may be accomplished by external or internal fixation.
(a) Methods of external fixation include casts, splints, and continuous traction.
(b) Internal fixation devices include pins, wires, screws, rods, nails, and plates. These devices, attached to the sides of the bone or inserted through the bone, provide internal immobilization of the bone.
(3) Rehabilitation. Rehabilitation is the regaining of strength and normal function in the affected area. Specific rehabilitation for each patient will be based upon the type of fracture and the methods of reduction and immobilization used. The physician will generally consult with the physical therapist to develop an individualized rehabilitation plan for each patient. This plan is normally implemented and controlled by the physical therapy department.
1-48. NURSING MANAGEMENT OF A PATIENT WITH A FRACTURE
a. Nursing care of a patient with a fracture, whether casted or in traction, is based upon prevention of complications while healing. By performing an accurate nursing assessment on a regular basis, the nursing staff can manage the patient’s pain and prevent complications.
b. When assessing a patient with a fracture, check the “5 P’s”–pain, pulse, pallor, paresthesia, and paralysis.
(1) Pain. Determine where the pain is located and if it is worse or better? Worsening pain may indicate increased edema, lack of adequate blood supply, or tissue damage.
(2) Pulse. Check the peripheral pulses, especially those distal to the fracture site. Compare all pulses with those on the unaffected side. Pulses should be strong and equal.
(3) Pallor. Observe the color and temperature of the skin, especially around the fracture site. Perform the capillary refill (blanching) test.
(4) Paresthesia. Examine the injured area for increase or decrease in sensation. Can the patient detect tactile stimulation such as a blunt touch or a sharp pinprick? Does the patient complain of numbness or tingling?
(5) Paralysis. Check the patient’s mobility. Can he wiggle his toes and fingers? Can he move his extremities?
c. All nursing assessment findings should be documented in the patient’s chart so that comparison can be made with notes made at both earlier and later dates. In this way, the patient’s progress can be followed and changes in status are easily recognized. In addition to the five P’s mentioned above, the patient’s level of consciousness and temperature should be checked regularly. Mental status changes and temperature elevation could indicate the presence of infection. Reposition the patient as necessary to relieve pressure areas. Check all dressings, bandages, casts, splints, and traction equipment to ensure that nothing is causing constriction or pressure. Frequent and thorough checking and observation on the part of the nursing staff will promote healing and prevent complications.
1-49. LIFE THREATENING COMPLICATIONS
a. Pulmonary Embolism. Pulmonary embolism is the occlusion of the pulmonary arteries by a thrombus originating in the venous system. Patients with lower extremity fractures are most susceptible to pulmonary embolism due to their relative inactivity. This condition may occur with or without symptoms. If symptoms do occur, they may present as substernal pain, dyspnea, apprehension, weak and rapid pulse, shock, or simply a subtle deterioration of the patient’s condition for no obvious reason. The treatment ordered by the physician will be symptomatic and normally involves the use of anticoagulant therapy and elastic stockings.
b. Fat Embolism. In fat embolism, fat droplets enter the circulatory system, obstructing blood flow and causing inflammatory reactions in the affected vessels. Onset usually occurs within 24-72 hours after injury. Fat emboli in the lungs may result in defective transfer of respiratory gases, causing dyspnea and air hunger. Some emboli may affect the central nervous system and cause restlessness and confusion. Again, treatment addresses the signs and symptoms. Oxygen is normally administered and, if necessary, the physician will order intubation and mechanical ventilation. Anti-inflammatory and diuretic medications will often be used as well.
c. Gas Gangrene. Gas gangrene is a severe infection of skeletal muscle caused by the bacteria Clostridium. These bacteria are anaerobes and spore formers normally found in soil and in the intestinal tract of man. Gas gangrene occurs most often in wounds that have been grossly contaminated at the time of injury, in wounds that have a small but deep open wound area, and in wounds that have a compromised blood supply and therefore a decreased oxygen supply. Gas gangrene causes production of toxins and decomposition of tissue. Necrotic tissue will produce gas bubbles, which are evidenced by crepitus (crackling) in the soft tissue, along with severe pain and edema. Nursing personnel should observe for signs of apprehension, fever, chills, increased pulse, increased respiratory rate, and frothy foul-smelling drainage from the wound. Strict nursing observation is critical for patients with susceptible wounds because gas gangrene will often progress to a severe stage deep in the tissue before any signs or symptoms become evident. In treating gas gangrene, the physician will open the wound for debridement and irrigation. Antibiotic therapy and hyperbaric oxygen therapy will be initiated. Frequently, amputation of the affected extremity is necessary.
d. Tetanus. Tetanus is an acute infection caused by the tetanus bacillus, another anaerobic spore former. The bacteria is introduced through a wound that has been contaminated with soil, feces, or dust. Toxins that have an affinity for nervous tissue cause hyperirritability, restlessness, muscle rigidity, and tonic muscular spasms of almost every muscle group. The patient may have difficulty opening the mouth due to spasm of facial muscles. Tetanus is sometimes referred to as “lockjaw” for this reason. Treatment is similar in nature to that of gangrene, with the addition of anti-convulsive drugs.
