3-1. INTRODUCTION
Ideally, a person gets the fluids and electrolytes needed to live by the oral route. This route has certain built-in safeguards against bacterial invasion. When the intravenous route of administration must be used, the material being given is injected directly into the circulatory system through the veins. Although, this route is certainly effective in terms of getting the fluid into the patient, the intravenous route is not completely safe. Complications (that is, infection) can happen. In the case of infection, the fluid being administered, the intravenous administration set (the equipment between the bottle or the bag and the patient), and the techniques used to start the fluid administration are possibilities for bacterial contamination. The intravenous administration of fluids is to be taken seriously.
3-2. INTRAVENOUS PREPARATIONS
You may have seen intravenous solutions being administered to a patient. The bottle or bag connected to the patient by a plastic tube means life to many patients.
a. Intravenous Solutions. Intravenous solutions are products that meet certain rigid requirements and are supplied ready for use by manufacturers. Examples of such intravenous solutions are five percent dextrose, 0.9 percent sodium chloride, and lactated Ringer’s. These solutions are ready for use as soon as they arrive from the manufacturer. You will see the lactated Ringer’s and the 0.9 percent sodium chloride used as “to keep open” (TKO) solutions. They serve as a ready and rapid way by which drugs could be given to the patient should the patient go into shock. These solutions serve as a “base” for the admixtures.
b. Intravenous Admixtures. Intravenous admixtures are intravenous solutions to which have been added one or more drugs. For example, it is common for a patient to be administered a liter of five percent dextrose which has 20 mEq of potassium chloride added to it. Thus, the patient received fluid, nutrients (dextrose), and electrolytes (potassium and chloride). Typically, patients receive much more complicated intravenous admixtures. These intravenous admixtures are usually prepared in the Pharmacy Sterile Products Section by specially trained personnel who use aseptic techniques. At times, it may be necessary for the physician or the person administering the infusion to add one or more drugs after the solution is already in place. This is done only on the physicians order.
3-3. CATEGORIES OF INTRAVENOUS FLUIDS AND THEIR USES
Many patients on the battlefield or in hospitals receive intravenous fluid therapy. They receive intravenous fluid therapy for many different reasons. All solutions received aren’t alike. Many patients have intravenous solutions tailored to meet their specific fluid, nutritional, and electrolyte needs, especially if they require long term intravenous therapy.
3-4. HYDRATING SOLUTIONS
a. Use. Hydrating solutions are used to provide the patient with required fluid that is, water). The volume of preparation administered depends on the fluid needs of the patient.
b. Examples. Below are some examples of preparations commonly used as hydrating solutions:
(1) Five percent dextrose solution. Five percent dextrose solution (D5W) consists of dextrose and water. One liter of the five percent dextrose contains approximately 170 calories. This solution contains no appreciable electrolytes. Therefore, electrolytes are sometimes added to the five percent dextrose solution (for example: Fifteen mEq KCL in one liter of D5W). The five percent dextrose solution is used to provide fluid replacement and energy. D5W is not commonly used in the level 1 treatment environment. NOTE: Dextrose solution is available in several concentrations.
(2) Nine-tenths percent sodium chloride solution (normal saline). This product is a solution of sodium and water. Each 100 milliliters of solution contains 0.9 gram of sodium chloride. Nine-tenths percent Sodium chloride solution contains 154 milliequivalents of sodium and 154 milliequivalents of chloride in each 1,000 milliliters of solution. This product is used to provide fluid replacement and to replace moderate losses of the sodium ion (Na+). Normal saline is often used in trauma patients as a volume expander before blood products are available. However, colloid solutions are preferred for volume replacement in trauma patients on the battlefield.
NOTE: Sodium chloride solutions are also available in other concentrations. For example, 0.45 percent sodium chloride solution is commonly seen.
(3) Five percent dextrose solution in 0.9 percent sodium chloride solution. This product has in each 100 milliliters, five grams of dextrose and 0.9 grams of sodium chloride. Not only does this product provide a source of fluid, it also serves as a source of both energy (170 calorie/liter) and sodium. This product is used in fluid replacement, in the replacement of moderate losses of sodium, and as a source of energy.
NOTE: Various combinations of dextrose and sodium chloride are available.
3-5. ELECTROLYTE REPLACEMENT SOLUTIONS
a. Use. Electrolyte replacement solutions provide both electrolytes (like sodium, potassium, and so forth) and fluid to the patient. Special electrolyte replacement solutions can be prepared in order to meet the needs of particular patients.
b. Examples of Electrolyte Replacement Solutions. Below are two of the solutions commonly used to replace electrolytes.
(1) Lactated Ringer’s solution (LR, Ringer’s lactate, RL, Hartmann’s solution). This product is a solution of electrolytes in water. This product contains sodium, potassium, calcium, chloride, and lactate ions. The lactate ion in the product has an alkalizing effect. The lactate ion is metabolized in the liver to glycogen and ends up as carbon dioxide and water. Lactated Ringer’s solution is used as a fluid replacement and as an electrolyte replacement. Lactated Ringer’s is the preferred solution for heat injuries.
(2) Lactated Ringer’s solution with five percent dextrose. This product is a combination of lactated Ringer’s solution and five percent dextrose (D5RL) solution. The dextrose supplies 170 calories per 1,000 milliliters of solution. Lactated Ringer’s solution with five percent dextrose is used as a fluid replacement, electrolyte replacement, and as a source of energy.
NOTE: Other combination products are available.
3-6. NUTRIENT SOLUTIONS (HYPERALIMENTATION PRODUCTS)
These products provide total parenteral nutrition for those patients who cannot, should not, or will not ingest the nutrients they need to live. It should be noted that a hyperalimentation solution can supply all the patient’s nutritional needs by administration through the circulatory system. However, these solutions are quite expensive and, because of their nutrient content, are highly susceptible to bacterial growth. Most of the solutions contain high concentrations of carbohydrates (for example, dextrose). Because of this high concentration, the solutions must be administered through a large-bore vein. Just placing the needle or catheter into such a large-bore vein is a surgical procedure in itself.
The hyperalimentation solution is prepared in the Pharmacy Sterile Products Section by a specially trained person. You must be very careful to prevent bacterial contamination. The preparation of the product itself is quite a job because the preparer must add ingredients in a certain sequence. Many of the components of a hyperalimentation solution are incompatible in certain concentrations. The components of most hyperalimentation solutions are water, dextrose, amino acids, electrolytes, and vitamins. One product, IntralipidR, is an oil in water emulsion. IntralipidR is one hyperalimentation product that can be administered through a small-bore vein such as those found in the arm.
3-7. REQUIREMENTS FOR INTRAVENOUS SOLUTIONS/INTRAVENOUS ADMIXTURES
Any solution administered through a patient’s veins must be:
a. Sterile. Sterile means that no living microorganisms are present in the solution.
b. Pyrogen-Free. Pyrogens are substances that produce fever when injected into the circulatory system.
c. Free from Visible Particulate Matter. Visible particles in an intravenous preparation mean that the product should be discarded. These particles could have been present in the solution when it arrived in the pharmacy or they may have been accidentally added to the solution when other substances were added. Regardless of origin, these visible particles, if intravenously administered, could cause a blockage in the patient’s circulatory system. Filters with very small pores are available which can remove these visible particles as the product is being administered. Remember, the origin of the particles is unknown-it is possible that some particles could be undissolved drug. Removing the drug particles would be good, but if the filtered particles are undissolved drug, by removing them you may be lowering the amount of drug in the solution.
3-8. PRECAUTIONS FOR USING FLUID THERAPY
You will likely be in a position to administer or supervise administration of fluid therapy. Some precautions will be beyond your control, but most will be your responsibility. Carefully watch for the pitfalls shown below, to make sure that the intravenous infusion does the patient more good than harm.
a. Contamination. A solution intravenously administered to a patient must be free from living microorganisms. You have a responsibility for using the aseptic technique. When there is doubt about the sterility of the admixture (or intravenous solution), the product should be discarded. Microorganisms are present in the environment of the hospital room. They are on the hands of the person who will start (that is, begin the administration) the intravenous product. Therefore, this person is responsible for using care and aseptic technique to make the venipuncture.
b. Irritating Drugs. The veins are very sensitive. Therefore, any intravenous product which has an extreme pH or which is very concentrated can irritate the veins. In some cases, the physician can decide to place the drug in another intravenous solution resulting in a pH that will not irritate the veins as much. In other cases, the site can be changed frequently to allow the part of the vein just used to recover.
c. Particulate Matter. Hold a bottle or bag of intravenous solution up in front of a light. See how it is sparkling clear. Actually, small particles called particulate matter are present in the solution. Standards allow extremely small particles to be present in the solution in certain concentrations. Intravenous solutions or admixtures should never be administered to a patient when the products contain visible particulate matter. A product that is cloudy might actually be cloudy because of suspended particulate matter. Even though filters are available which can filter most particulate matter from intravenous products, do not use a cloudy solution.
3-9. SITE FOR VENIPUNCTURE
a. Selection. Site selection for venipuncture depends on:
(1) Accessibility of the vein. A vein should be relatively easy to feel and to stabilize for venipuncture. If this task is too difficult, select another vein.
(2) General condition of the vein. If the vein is in good condition, it will easily take the venipuncture. If the vein is poor, it may collapse upon puncture.
(3) Type of fluid to be infused. If the fluid used is especially irritating, a different site will be suitable from the sites, which can be used for non-irritating fluids.
(4) Period the intravenous line is expected to be in place. Long-term intravenous therapy will often require a different site from the ones that can be used if a single bottle or bag of fluid will be used.
b. Preferred Sites. The following sites are generally used and preferred for use by most physicians in the clinical setting it is possible to select preferable veins for puncture. On the battlefield and keeping with the tenants of Tactical Combat Casualty Care (TC3), you should puncture a high percentage vein such as antecubital or external jugular.
(1) Distal to the antecubital area (that is, cephalic, basilic, antebrachial veins in the lower arms).
(2) Veins on the back of the hand.
(3) Veins in the lower extremities when necessary although danger of thrombophlebitis is considerably greater.
(4) The leg and foot veins may be used on children because these vessels are not sclerosed.
CAUTION: Select the largest vein, if possible, when injecting intravenous drugs that may produce sloughing/necrosis injury to the tissues.
(5) Scalp veins are used in infants.
3-10. PRINCIPLES OF INTRAVENOUS THERAPY
a. Check all bottles or bags of infusion solution for these specific requirements and discard any that show:
(1) A broken vacuum seal.
(2) Cloudiness.
(3) Precipitation (particles on the bottom of the bag or bottle).
(4) Foreign contaminants.
b. Always, use sterile equipment and wash your hands thoroughly.
c. Disinfect the patient’s skin at and around the injection site. Apply antiseptic solution using friction at and around the venipuncture site.
d. For long term therapy patients.
(1) Change the injection site every 48 to 72 hours (to lessen the possibility of infection and/or irritation to the vein), or in accordance with (IAW) local standing operating procedures (SOP).
(2) Replace the tubing and solution bottle (or bag) every 24 hours (to avoid infusing a contaminated solution) or IAW local SOP.
(3) Take precautions if vein irritation or thrombophlebitis is possible.
(a) Plastic catheters are more likely to cause irritation than stainless steel needles.
(b) Use the smallest gauge needle or catheter possible.
(c) Use the shortest infusion time possible. Irritation is much more likely after 48 hours of intravenous therapy.
(d) Veins of the lower extremities (in adults) are more likely to develop phlebitis (and quicker) than those of the upper extremities.
(e) Do not irrigate a stopped infusion. You may dislodge an obstructive clot and endanger the patient’s life.
(f) You are less likely to irritate the large veins of the central venous system than the smaller peripheral veins.
(g) Strict attention to aseptic techniques is required at all times to prevent sepsis.
3-11. COMPLICATIONS
The complications of intravenous therapy may be mild or life threatening, but they are always uncomfortable for the patient. Many can be prevented with proper care.
a. Infiltration. Infiltration (the most frequent complication) is caused by dislodgement of the needle or catheter or by puncture of the vein. This allows the fluid to collect in the surrounding tissue. Signs or symptoms include, slowing or stopping of the intravenous flow and reduced skin temperature in the venipuncture area. This is not usually serious but can be very uncomfortable for the patient. You can restart the intravenous at another site. The danger of this happening can be reduced by securely taping the intravenous line and providing arm boards for stability.
b. Speed Shock or Circulatory Overload. The “average” person has a blood volume of about five to six quarts. Blood is approximately ninety-one percent fluid. The body has intricate mechanisms for making up for changes in blood volume. For example, when you donate blood, some fluid from the inside of the cells and fluid surrounding the cells enters the circulating blood volume. There is a reverse flow when the blood volume is normal and intravenous fluids are administered. Unfortunately, when too much fluid and/or too much medication is administered too rapidly, circulatory overload can result. Signs and symptoms include patient complaints of pounding headache and chills, a flushed look, irregular pulse, and dyspnea.
c. Sepsis and Pyrogenic Reactions. Sepsis and pyrogenic reactions are usually caused by the introduction of pyrogenic organisms or their toxins into the bloodstream. In addition to these organisms, febrile reactions can be caused by various chemicals and certain types of particles. If an infection results, the reaction can be localized or systemic. A systemic reaction can occur about thirty minutes after starting the intravenous infusion. Long-term therapy patients can develop sepsis from the growth of microorganisms on the skin after a two to three day period. Signs and symptoms include an unexpected rise in temperature preceded by chills, nausea, vomiting, backache, and malaise. To reduce the possibility of developing sepsis, use aseptic techniques when starting the infusion and change the infusion site, bottle, and tubing at least every two to three days on long term intravenous therapy patients.
d. Phlebitis. Phlebitis is an irritation or injury to the vein. It can be caused by mechanical, chemical, or bacterial irritation. Signs and symptoms include redness, pain, and swelling at the infusion site and patient complaints of fatigue together with fever and a rapid pulse. If signs appear, change the needle to another site and apply warm moist compresses to relieve discomfort and aid healing. Do not rub or massage the affected area. You could cause thrombus or emboli and add to the vein damage. A thrombus is a clot that is formed in the blood vessels. A thrombus is usually a further complication of phlebitis. A clot formed in the vessels can produce damage to tissue below the stoppage.
e. Air Embolism. An air embolism is a very serious intravenous therapy complication. It can occur when a sizeable amount of air gets into the circulatory system through the intravenous administration set. It can block a vessel so that tissues are unable to get oxygen. Nutrients and waste products cannot be removed. The air bubble can cut off cardiac, cerebral, or pulmonary circulation. Symptoms include a fall in blood pressure, tachycardia (rapid pulse), and loss of consciousness. If a patient has these symptoms, take his vital signs, place patient on his left lateral side, administer oxygen, and get immediate medical help. Air embolism can be prevented by removing all air (bleeding) from intravenous lines, using venipuncture sites below heart level, and never allowing an intravenous line to run dry before disconnecting or adding another bottle. The larger the embolus, the greater the danger. Death could result.
f. Solution’s Incompatibility. The signs of incompatibility will differ according to the solution or drug being administered. The effects can vary from neutralizing the effects of a drug to causing circulatory collapse. Some solutions, such as over 10 percent dextrose or potassium chloride, are very irritating in concentrated doses. Sterile water, saline, or special dilutants are required for certain drugs and substitutions should not be made. Incompatible drugs frequently form a precipitate and cause fever, nausea, vomiting, and intense itching.
3-12. CALCULATING THE INTRAVENOUS DRIP RATE
In order to infuse a solution ordered by the physician, it is necessary to calculate the infusion rate. A drip rate calculation may be desired for maintenance of trauma patients that you may not be able to immediately evacuate. During the care under fire phase of tactical care the appropriate hypovolemic fluid protocols should be followed for the benefit of your patient and triage of your available supplies.
a. The physician who ordered the infusion for the patient will give you the following information:
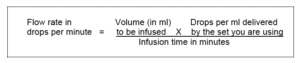
b. From the infusion set, you will learn how many drops per ml the set is capable of providing. You must determine how many drops per minute are required in order to set this delivery rate on the infusion set. The formula for determining the drip rate is given below.
(1) The type or kind of fluid to be infused.
(2) The amount of fluid to use.
(3) The time period over which the total amount of fluid is to be infused.
3-13. EXPLANATION OF DRIP RATE FORMULA
The above formula can be used by following these steps.
a. Multiply the number of ml to be infused (ordered by the physician) by the drops per ml delivered by the set you are using (shown on the infusion set).
b. Multiply the hours of infusion time (ordered by the physician) by 60 minutes.
c. Divide the answer in step number one by the answer in step number two. This answer will be the flow rate.
3-14. EXAMPLE OF A DRIP RATE CALCULATION
Let us use an example to illustrate this process. The physician has ordered you to infuse 2000 ml of normal saline. The fluid is to be infused over eight hours. Your infusion set delivers 15 drops per milliliter. How many drops per minute should be administered?
a. Multiply 2000 ml by 15 drops per ml. Answer: 30,000 drops.
b. Multiply 8 hours by 60 minutes. Answer: 480 minutes.
c. Divide 30,000 by 480. Answer: 62 drops per minute.