LESSON 2 Heart Attack and Cardiopulmonary Resuscitation.
TEXT ASSIGNMENT Paragraphs 2-1 through 2-9.
LESSON OBJECTIVES After completing this lesson, you should be able to:
2-1. Define clinical death, biological death, heart attack, cardiac arrest, and cardiopulmonary resuscitation.
2-2. Identify factors that increase a person’s risk of having a heart attack.
2-3. Identify signs and symptoms of a heart attack.
2-4. Identify how cardiopulmonary resuscitation simulates normal breathing and heartbeat.
2-5. Identify the recovery rates for cardiopulmonary resuscitation.
SUGGESTION After you have completed the text assignment, work the exercises at the end of this lesson before beginning the next lesson. These exercises will help you to achieve the lesson objectives.
2-1. DEFINITIONS
a. Heart Attack. A heart attack (myocardial infarction) is the death of heart muscle tissue caused by a blood clot (thrombus) or other substance circulating in the blood (embolus) that blocks one or more of the coronary arteries (arteries that provide the heart muscles with oxygen-rich blood).
b. Cardiac Arrest. Cardiac arrest (sudden death) is the sudden and unexpected cessation of pulse and blood circulation. That is, the casualty’s heart stops beating. When the heart stops beating, the casualty’s breathing will also stop and he will loose consciousness, usually within 10 to 30 seconds of the cardiac arrest.
c. Clinical Death. Clinical death occurs as soon as the casualty’s heart stops beating, he stops breathing, and he looses consciousness. Clinical death can be reversed by cardiopulmonary resuscitation (CPR).
d. Biological Death. Biological death usually occurs 6 to 10 minutes after clinical death if efforts to restore breathing and heartbeat are not performed. Biological death involves irreversible brain damage.
e. Cardiopulmonary Resuscitation. The prefix “cardio-” refers to heart, “pulmonary” refers to the lung, and “resuscitation” means to bring a person who appears to be dead back to consciousness. Thus, cardiopulmonary resuscitation means to restore lung function (breathing) and heart function (blood circulation) to a person who is clinically dead.
2-2. CAUSES OF CARDIAC ARREST
The primary cause of sudden death (cardiac arrest) is myocardial infarction (heart attack). Other causes of cardiac arrest include:
a. Drowning.
b. Electrical shock.
c. Poisoning
d. Suffocation.
e. Smoke inhalation.
f. Choking on food or other objects.
g. Anaphylactic shock (shock caused by hypersensitivity [severe allergic reaction] to a substance such as the venom from a bee sting).
h. Trauma (major injury).
i. Medical reasons (terminal illness, septic shock, sudden infant death syndrome, and so forth).
j. Hypovolemic shock (shock caused by severe blood loss).
k. Drug reaction.
2-3. PREDISPOSING FACTORS OF HEART ATTACK (RISK FACTORS)
Disease related to the heart and blood vessels are the greatest killers of people in this country.
According to a 2005 American Heart Association study, sudden cardiac death from coronary heart disease occurs over 900 times per day in the United States. The risk in adults is estimated to be about 1 per 1,000 adults 35 years of age and older per year. Sudden cardiac death in the young (people less than 35 years old) is much less common than in older adults, occurring in only 0.5 to 1 per 100,000 per year.
A review of published studies that report initial heart rhythms during cardiac arrest in children indicates that the majority (40 to 90 percent) of children have asystole (a-SIS’to-le) or pulseless electrical activity when first evaluated. However, ventricular fibrillation or ventricular tachycardia (ven-TRIK’u-ler tak”eh-KAR’de-ah) is found in about 7 to 14 percent of all children in cardiac arrest in the prehospital setting.
About 60 to 70 percent of people who suffer myocardial infarction (MI) die before they reach a hospital. Most deaths from myocardial infarction occur within 2 hours following the heart attack. Death is usually caused by cardiac dysrhythmia (ventricular tachycardia), in which abnormal heart contractions prevent the normal circulation of blood. Some of the predisposing factors (those factors which make an incident more likely to occur) associated with heart attacks can be controlled. Controlling these factors makes a person less likely to have a heart attack.
a. Major Risk Factors. The four most important factors that predispose to heart attacks are listed below. All of these factors can be controlled.
(1) Cigarette smoking. A person who smokes more than one pack of cigarettes a day is twice as likely to have a heart attack than is a nonsmoker.
(2) Elevated (high) blood pressure. A person with a systolic pressure over 150 has more than twice the risk of heart attack (and four times the risk of stroke) than a person with a systolic pressure under 120. A diastolic pressure over 90 also increases the risk of heart attack.
(3) Elevated blood cholesterol. A person with a blood cholesterol level of 250 milligrams per deciliter (mg/dl) or higher has a greater risk of heart attack than does a person with normal blood cholesterol level.
(4) High fat, high cholesterol diet. A person who eats large amounts of foods that are high in fat and cholesterol runs a greater risk of heart attack than does a person who eats a normal diet.
b. Other Risk Factors. The following are also risk factors that, for the most part, are beyond the person’s control.
(1) Age. Older persons are more likely to have heart attacks. About one-fourth of all heart attacks, however, occur in individuals under the age of 65.
(2) Sex. Males are more likely to have heart attacks than females.
(3) Diabetes. Diabetes increases the risk of heart attack; however, the risk may be lessened through medication and diet.
(4) Heredity. A person whose family has a history of cardiovascular disease is at greater than normal risk.
c. Unproven Factors. Some factors which are thought to make a heart attack more likely, but are not yet proven to do so, are:
(1) Obesity.
(2) Certain personality types.
(3) Stress.
(4) Lack of regular exercise (physical hypoactivity).
2-4. SIGNS AND SYMPTOMS OF A HEART ATTACK
A myocardial infarction can happen to either males or females, old or young, and not necessarily during physical or emotional stress. A person experiencing the early signs and symptoms of a heart attack may not know that he is having a heart attack. He may state that he feels like having “bad indigestion.”
a. A heart attack may begin with pain, uncomfortable pressure, squeezing, fullness, or tightness around the chest. The pain is usually located in the center of the chest behind the breastbone (sternum). The pain may be substernal and may be described as crushing; many patients describe the pain as, “It feels like an elephant is sitting on my chest.” The pain may not be severe. Sharp, stabbing twinges of pain are usually not symptoms of a heart attack.
(1) The pain may spread to a shoulder, an arm, or neck.
(2) The duration of the pain is usually 2 minutes or longer. The pain may come and go.
b. The person may also feel weak, have shortness of breath, perspire, and be nauseous (feel like vomiting).
c. Signs and symptoms may come and go, depending upon factors such as the severity of damage to the casualty’s heart and the casualty’s physical activity during or immediately before the heart attack. The disappearance of symptoms may cause the casualty to deny that he has suffered a heart attack.
d. In some cases, the heart attack results in cardiac arrest (no pulse or heartbeat).
2-5. NEED FOR CARDIOPULMONARY RESUSCITATION
As stated previously, the blood supplies the cells of the body with oxygen. In a medical emergency, you must ensure that this supply of oxygen continues. The supply of oxygen to the body cells is threatened whenever the person stops breathing on his own or when the person’s heart stops pumping blood. When the oxygen supply fails, cells begin to die.
The length of time required for a cell to die after the oxygen supply has stopped depends upon several factors. One of the most important factors is the type of cell involved. Brain cells are the most sensitive. Permanent brain damage usually occurs if the oxygen supply is stopped for more than 6 minutes. Therefore, a casualty who has suffered a cardiac arrest must have breathing and circulation restored quickly if biological death is to be prevented. The process of restoring breathing is called rescue breathing. Artificial heartbeats are produced by administering chest compressions. In neither case, however, is the substitute measure as efficient as the body’s natural process.
2-6. EFFECTS OF RESCUE BREATHING
Rescue breathing consists of two phases. In the first phase, the rescuer blows a breath into the casualty’s lung. This replaces the casualty’s normal inhalation. Once the inhalation phase is completed, the rescuer breaks his seal over the casualty’s airway. This allows the casualty’s body to exhale on its own.
a. Inhalation Phase. Once the rescuer seals the casualty’s airway so that air cannot escape, he blows air into the casualty’s airway (usually though the casualty’s mouth). The pressure from the rescuer’s breath forces air through the rest of the respiratory tract and causes the alveoli to expand. This causes in the lungs as a whole to expand. When the lungs expand, they cause the rib cage (chest) to rise and the diaphragm to flatten somewhat.
b. Exhalation Phase. When the rescuer removes his mouth from the casualty (breaks the seal over the casualty’s airway), the higher air pressure in the casualty’s respiratory system causes air to rush from the airway and into the atmosphere. The rib cage and the diaphragm resume their normal positions (the chest falls and the diaphragm pushes into the chest cavity by resuming its dome-like shape). These actions result in air being forced out of the lungs, just as in normal exhalation.
2-7. EFFECTS OF CHEST COMPRESSIONS
a. The heart is located between the sternum and the spine. If the sternum is pressed down (depressed) far enough into the chest cavity (1 1/2 to 2 inches in an adult), the heart is compressed between the sternum and the spine (figure 2-1A). Blood is then forced out of the ventricles and into the arteries.
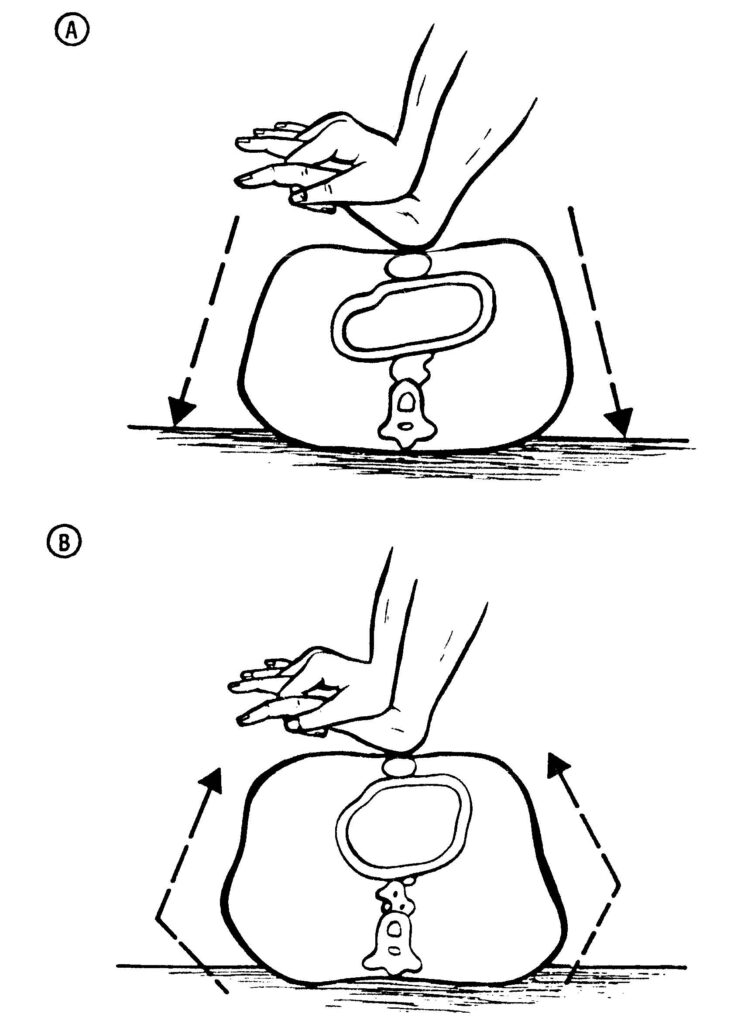
A Compression.
B Release.
b. When the pressure is removed from the sternum, it rises to its normal position and the heart resumes its normal shape (figure 2-1B). Since blood was forced out of the ventricles during the compression, blood flows from the atria into the ventricles, as the heart returns to its normal shape. As blood flows out from the atria into the ventricles, blood also flows from the veins to refill the atria.
c. Each pressure-release cycle is roughly equal to one heartbeat.
2-8. ROLE OF THE RESCUER
In order to properly treat a casualty requiring CPR, the rescuer must take the following actions. These actions are summarized in figure 2-2.
a. Early Access. The rescuer, whether trained or untrained, must activate the emergency medical service (EMS) system early, even before beginning CPR.
b. Early CARDIOPULMONARY RESUSCITATION. The brain and other body tissues cannot tolerate long term hypoxia (low state of oxygen in the blood). Because of this, CPR must be started as soon as possible to increase the chance of patient survival. High-quality bystander CPR can double or triple survival rates from cardiac arrest. Less than one-third of victims of sudden cardiac arrest (SCA) receive bystander CPR, and even fewer receive “high-quality” CPR.
c. Early Defibrillation. Treatment of ventricular fibrillation (VF) in SCA requires early CPR and shock delivery with a defibrillator. Lay rescuer and first responder CPR and automated external defibrilator (AED) programs in airports and casinos and with police officers have reported survival rates from witnessed VF SCA as high as 49 to 74 percent.
d. Early Advanced Care. Early Advanced Cardiac Life Support (ACLS) procedures should be performed.

2-9. RECOVERY RATES
Experience with situations requiring basic life support (BLS) has demonstrated that a significant number of casualties suffering cardiac arrest can be successfully resuscitated if CPR is provided promptly and followed by more advanced cardiac life support. Prompt response is critical.
a. Early CPR and defibrillation within the first 3 to 5 minutes after collapse, plus early advanced care can result in high (greater than 50 percent) long-term survival rates for witnessed ventricular fibrillation.
b. The value of early CPR by bystanders is that it can “buy time” by maintaining some blood flow to the heart and brain during cardiac arrest. Early bystander CPR is less helpful if EMS personnel equipped with a defibrillator arrive later than 8 to 12 minutes after the collapse.